Maintaining a normal blood pressure is vital for all body systems. High blood pressure can cause organ damage or a stroke while extremely low blood pressure can cause someone to go into shock.[1]
This is why accurate blood pressure monitoring is important when caring for patients.
Invasive blood pressure monitoring measures arterial pressure via arterial cannulation and is most often used during surgery and with critically ill patients to provide continuous readings.
Noninvasive blood pressure (NIBP) monitoring can be either intermittent or continuous. The most common is intermittent via an inflatable cuff that occludes the arm to measure pressure.[2] Intermittent NIBP can be done manually by auscultating for Korotkoff sounds (or palpating pulse) or with a machine using oscillometry.
Continuous NIBP can be done in a few different ways, older methods include using the volume clamp method or arterial applanation tonometry.2 Pulse wave transit time is also used and typically involves using a pulse oximeter and ECG. [3]
The most recent promising method is called pulse wave analysis (PWA) or pulse wave decomposition (PWD) that estimates continuous NIBP from optical plethysmographic signal or from a finger cuff.[4]
There are pros and cons to both invasive and noninvasive blood pressure monitoring. Invasive monitoring using an arterial line tends to be more accurate but carries an increased risk of infection, bleeding, and blood clot formation.[5]
NIBP monitoring eliminates those risks but has been found to be less accurate than using arterial access.4
The two commonly known values that make up a blood pressure reading are systolic (SYS) and diastolic (DIA) pressures. Systolic is the maximum arterial pressure during contraction of the left ventricle of the heart, while diastolic is the minimum arterial pressure during relaxation and dilatation of the ventricles of the heart.[6]
There is another measure calculated from the systolic and diastolic readings and that’s the mean arterial pressure (MAP) which is the average pressure throughout one complete cardiac cycle.[7] In order to determine MAP, there is a specific MAP calculation that is typically included with a NIBP reading using a mechanical device.
Today we’re going to discuss how to calculate mean arterial pressure and its significance.
BP cuff size matters
In order to determine the MAP, you need a general blood pressure reading first to determine systolic and diastolic measurements. This is typically done with a blood pressure cuff either manually or using medical equipment such as, the CARESCAPETM V100 or CARESCAPE VC150 vital signs monitors.
Oscillometric devices, such as the CARESCAPE V100 or CARESCAPE VC150 vital signs monitors with DINAMAP SuperSTAT NIBP algorithm, calculate MAP from the pressure waveform, and results in a more accurate value compared to just calculating based on DIA and SYS.[8]
Since blood pressure readings are influenced by many variables, it’s important to account for as many as possible.
One of these variables is using the right cuff size.4 Cuff size is determined by looking at the circumference of the mid-arm and if the wrong size is used, it can skew blood pressure readings by up to 30 mmHg.[9]
According to the American Heart Association, a properly fitting blood pressure cuff has a width that is at least 40% and a length that is 80% of arm circumference. GE HealthCare NIBP cuffs come in several sizes to properly fit different sizes:
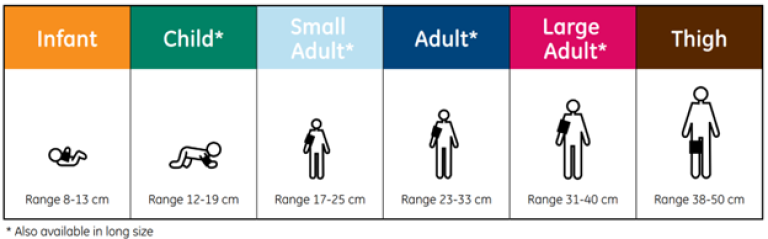
For example, if someone has an arm circumference ranging between 23-33 cm, they should use the regular ‘adult’ size of 16 x 30 cm.[1]
In order to ensure a proper cuff size is selected, the index line should fit within the marked range on the cuff.
When placing the cuff, the artery indicator should be placed over patient´s brachial artery. Make sure to wrap the cuff firmly around the patient´s arm, allowing for two fingers between the patient and the cuff.
MAP measurement
Automated MAP measurements using the oscillometer method use proprietary algorithms when calculating MAP.[2]
MAP is calculated using the following equation:
MAP = Diastolic BP + 1/3 x (Systolic BP – Diastolic BP)
MAP calculated with this formula is an estimation that might not be accurate when the pressure pulse shape of the patient is atypical, for example when measuring NIBP of a neonate. Automated MAP calculation with the oscillometric method is always recommended instead, when available.
What is a normal mean arterial pressure?
A normal MAP is between 70 and 100 mmHg.[3]
If the MAP drops below 60 mmHg, there is a concern there won’t be enough pressure to perfuse vital organs including the brain.6
If the MAP is above 100 mmHg, the patient may be experiencing a high artery pressure. The high pressure experienced in the arteries may lead to blood clots or heart muscle damage. 12
Why is mean arterial pressure important?
MAP provides the pressure throughout one complete cardiac cycle and is influenced by two variables:
- Cardiac output
- Systemic vascular resistance
In addition to the cardiovascular system, MAP is affected by the renin-angiotensin-aldosterone system in the kidneys as well as the autonomic nervous system through baroreceptors.6
While systolic and diastolic blood pressures are helpful indicators of hemodynamic changes including stroke volume and organ perfusion, they don’t provide a glimpse into cardiac output.[4]
Cardiac output helps determine flow rate, and how well blood is flowing determines how well tissue and organs are perfused. This illustrates the value of monitoring cardiac output with a noninvasive measure like MAP.11
MAP readings have been shown to be a useful independent predictor of several disease processes including metabolic syndrome and cardiovascular diseases. Cardiovascular mortality is also associated with MAP.[5]
In addition to providing information about the patient’s cardiovascular status, MAP readings tend to be more accurate than systolic blood pressure when using NIBP methods.
It’s well-known that systolic blood pressure NIBP values can vary due to multiple variables (including cuff size). Studies have shown hypotensive readings are overestimated, and hypertensive ones are underestimated.[6]
Clinicians are aware of the limitations of using noninvasive methods to monitor blood pressure. When surveyed, 47% of critical care intensivists used upper arm blood pressure readings to guide vasopressor therapy. 13
However, MAP measurements are consistently accurate when blood pressure is in a normal range.13
Summary:
- Blood pressure readings provide valuable information on patient status
- Noninvasive blood pressure measurements are commonly used, especially in noncritical settings
- Mean arterial pressure (MAP) provides additional information about perfusion and cardiac output status
- MAP calculations may also be a useful predictor of cardiovascular disease and cardiovascular mortality
- MAP measurements can be more accurate than systolic readings
References
[1] Centers for Disease Control and Prevention. (2022). About high blood pressure. https://www.cdc.gov/bloodpressure/about.htm accessed Dec. 20, 2022.
[2] Meidart, A. & Saugel, B. (2017). Techniques for non-invasive monitoring of arterial blood pressures. Frontiers in Medicine. 4:231.
[3] Smith, et al. (1999). Pulse transit time: an appraisal of potential clinical applications. Thorax, 54:452-457.
[4] Wilkison, I, Cockcroft, J, & Webb, D. (1998). Pulse wave analysis and arterial stiffness. J Cardiovasc Pharmacol. 32. Suppl 3:S33-7.
[5] Kaufmann, T et al. (2020). Non-invasive oscillometric versus invasive arterial blood pressure measurements in critically ill patients: a post hoc analysis of a prospective observational study. Journal of Critical Care. 57:118-123.
[6] Saad, R, Hasmi, M, & Nelson, V. (2022). Blood pressure measurement. National Library of Medicine: StatPearls.
[7] DeMers, D & Wachs, D. (2022). Physiology, mean arterial pressure. National Library of Medicine: StatPearls.
[8] https://clinicalview.gehealthcare.com/white-paper/dinamap-superstat-nibp-algorithm-carescape-patient-data-module
[9] Manning, D.M., et al. (1983). Miscuffing: Inappropriate blood pressure cuff application. Circulation 68(4), 763-6.
[10] Pickering, T et al. (2007). Recommendations for blood pressure measurement in humans: an AHA scientific statement from the council on high blood pressure research professional and public education subcommittee. The Journal of Clinical Hypertension. 7(2):102-109.
[11] Kiers, H et al. (2008). Oscillometric blood pressure measurements: differences between measured and calculated mean arterial pressure. The Netherlands Journal of medicine, 66(11):474-479.
[12] Meng, L et al. (2018). Blood pressure targets in perioperative care. Hypertension. 72:806-817.
[13] Sun, J, Yuan, J, & Li, B. (2021). SPB is superior to MAP to reflect tissue perfusion and hemodynamic abnormality perioperatively. Frontiers in Physiology. 12:705558.
[14] Fei, Y. Understanding the association between mean arterial pressure and mortality in young adults. Postgraduate Medical Journal. 96(1138):453-454.
[15] Meidert, A & Saugel B. (2017). Techniques for noninvasive monitoring of arterial blood pressure. Frontiers in Medicine. 4:231.








