Enhancing patient comfort and NIBP performance in challenging areas
Andrea Stebor, ARNP, PhD
Introduction
Health care providers today face an ever-changing and increasingly more challenging environment in which to provide patient care. What has not changed is the importance of obtaining quick and reliable patient data from which to make critical healthcare decisions. DINAMAP™ SuperSTAT, an advanced NIBP algorithm from GE Healthcare, can increase the overall speed and comfort of NIBP determinations, while maintaining a high standard of accuracy. The SuperSTAT algorithm can be found in the CARESCAPE™ Patient Data Module.
How is SuperSTAT different from the previous NIBP algorithms?
Traditional oscillometric automatic NIBP devices use a number of signal processing techniques to obtain accurate readings during a determination. These devices generally recognize pulses if they are equivalent in size at a cuff pressure and occur regularly in time. Additionally, the algorithms contained within these devices generally use a large number of deflation steps (typically 10-12 deflation steps) to help ensure accuracy. As a result, the traditional devices typically take some time to process the signals in order to determine the blood pressure (BP), particularly in the presence of arrhythmias or motion. The SuperSTAT algorithm uses advanced patented signal processing to address these deficiencies and can provide an accurate NIBP determination in as few as four pressure steps (however, as noted below, the initial SuperSTAT determination on a given patient will be very similar to a standard DINAMAP determination). A faster determination may result in a more comfortable determination for the patient. The SuperSTAT algorithm has been documented to improve speed, comfort and artifact rejection, while retaining the classic DINAMAP accuracy.
What are the enhancements in SuperSTAT NIBP?
Accelerated determinations
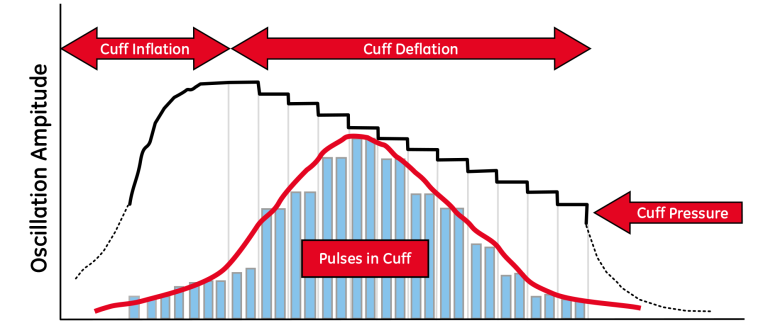
SuperSTAT NIBP uses “smart cuff” pressure control to face the challenge of providing accurate readings in a timely manner. The oscillometric method of determining NIBP is accomplished by a sensitive transducer, which measures cuff pressure and small pressure oscillations within the cuff. see Figure 1. A traditional determination (such as with the DINAMAP Classic algorithm) typically takes 10-12 deflation steps, while an accelerated determination with the SuperSTAT algorithm can take as few as four deflation steps -- which can result in a quicker determination.
The initial SuperSTAT NIBP determination will typically be as long as a traditional DINAMAP determination; this initial determination is called a learning determination because the algorithm is establishing the shape of the patient’s oscillometric envelope and storing the pattern of the patient’s oscillation (size) as a function of pressure. On each subsequent determination, the SuperSTAT algorithm can use information from the previous determination to perform smart cuff pressure control and select optimal pressure steps. During these subsequent determinations, the algorithm constantly evaluates data in an attempt to perform the determination in the shortest possible time. As a result, subsequent determinations with the algorithm will generally be shorter in length (accelerated determinations) unless the oscillometric data are found to be “noisy” or the patient’s BP has changed significantly.
Lower initial inflation pressures for neonates
Higher acuity in the Neonatal Intensive Care Unit (NICU) typically results in more neonates with low blood pressures. In the CARESCAPE Patient Data Module, the neonatal target inflation pressure for SuperSTAT NIBP can be set below the default target inflation pressure of 100 mmHg. With the SuperSTAT algorithm the clinician can set the neonatal target cuff inflation pressure to a minimum of 70 mmHg, which can provide more individualized NIBP inflation for the neonate with lower systolic BP, which may be more comfortable for the neonate with lower systolic BP.
Determination during irregular cardiac rhythms (in adult and pediatric patients)
Non-invasive monitoring techniques are continually challenged when attempting to acquire reliable NIBP readings on patients with irregular cardiac rhythms. Attempts to acquire NIBP readings in these circumstances often result in either a non-determination or multiple determination attempts. In patients with irregular cardiac rhythms, the pulse period and amplitude of the pressure pulses are constantly changing. In a traditional NIBP algorithm, this inconsistency in the cuff pressure waveform may cause it to be discarded as though it were artifact. When ECG is monitored, SuperSTAT NIBP can generally determine NIBP in the presence of irregular heart rhythms.
The SuperSTAT NIBP algorithm uses the ECG signal as an independent measure of pulse rate. At the beginning of a SuperSTAT NIBP determination, the coefficient of variation from the previous 120 R-R intervals is used to determine if an irregular rhythm is present. When the pulse rate varies outside of a predetermined range, the criteria for matching two BP oscillations will change. With the SuperSTAT algorithm during irregular rhythms, only pulses from the current determination are used in calculating the NIBP values. In order to provide for adequate artifact rejection capability and an increased likelihood of obtaining an NIBP determination, several criteria used to match and qualify the oscillometric pulses at each pressure step are relaxed and supplemented with additional information from ECG. Additional information from the ECG QRS complex and the pressure pulse are used to reject noise and include only physiologic oscillations. This process allows the algorithm to provide NIBP determinations in patients with irregular cardiac rhythms.
Motion artifact rejection
Motion artifact has always been an obstacle to obtaining accurate NIBP readings. In post-anesthesia care, the patient is often still under the influence of anesthetic drugs that may cause unexpected movements. In addition, motion also presents an inherent challenge when monitoring neonates, especially when BP signals are small, as is often the case in the NICU. The SuperSTAT algorithm assesses the presence and level of motion artifact by measuring the consistency of the pulse shape using several patented algorithms. Measuring the consistency of the pulse shape contributes to determining accurate NIBP values, even in the presence of motion artifact.
Larger performance range
Higher acuity hospitalized patients means greater variability in vital signs and greater challenges to obtaining NIBP values. For example, the pulse signals from patients with poor perfusion and small Neonates (premature infants weighing less than 1000 g) may be low and sometimes more difficult to measure with traditional BP technology. The SuperSTAT algorithm’s digital signal processing algorithms provide enhanced sensitivity (when compared to traditional BP technology) and as a result, can generally detect NIBP values on much smaller signals, such as in patients with low perfusion pressures.
Management of re-pumps and search capability
If, after an initial inflation and deflation, there are not enough data to determine an NIBP, the system re-inflates the cuff, typically to a higher cuff pressure. This process of re-inflating the cuff is known as a “re-pump” and the search process is known as its “search capability”. During the process of stepped deflation with the SuperSTAT algorithm, the oscillations at each of the pressure steps are stored. Unlike traditional oscillometric automatic NIBP devices, the SuperSTAT algorithm does a “smart search” by using previously stored oscillations to selectively “re-pump” as may be required, sometimes only to a single cuff pressure, to make an NIBP determination.
Frequently asked questions
What validation was done on SuperSTAT?
Accuracy of the SuperSTAT NIBP algorithm was validated in adult, pediatric, and neonatal subjects according to a national standard (ANSI/AAMI SP 10, 1992). The adult and pediatric studies were performed in cardiac catheterization lab areas and the neonatal studies were performed in NICUs. The reference standard of intra-arterial BP (IBP) was compared to the SuperSTAT NIBP values. The differences between the SuperSTAT NIBP readings and the IBP readings for systolic, diastolic, and mean arterial pressure (MAP) were analyzed. SuperSTAT NIBP readings were well within the national standard accuracy specifications of ±5 mmHg mean difference and less than or equal to 8 mmHg standard deviations for the adult, pediatric, and neonatal populations. The results of another neonatal study using SuperSTAT NIBP can be found in the peer review publication by Nelson, et al (2002).
Why does the SuperSTAT algorithm work well with neonates?
Some of the keys to getting accurate blood pressure determinations in the neonatal population include minimizing the cuff inflation time and rejecting motion artifact. The SuperSTAT algorithm incorporates these features to increase the likelihood of delivering reliable NIBP values. In addition, because of its enhanced sensitivity, the algorithm is able to obtain blood pressures in neonates who have very low perfusion pressures.
References
Levy S. et al. Atrial fibrillation: Current knowledge and recommendations for management. European Heart Journal 19, 1294-1320 (1998).
Cleland M.J. et al. Influence of arrhythmias on accuracy of non-invasive blood pressure monitors. Can J Anesth July;45(7), 699-705 (1998).
Eckert S. and Gleichmann U. Automated blood pressure measurement in special situations: Patients with chronic atrial fibrillation or chronic aortic regurgitation. Z Kardiol, 85 Suppl 3, 92-8 (1996).
Sykes D. et al. Measuring blood pressure in the elderly: Does atrial fibrillation increase observer variability. BMJ 300(6718), 162-3(1990).
Stewart M. et al. The accuracy of automated blood pressure measuring devices in patients with controlled atrial fibrillation. Journal of Hypertension 13, 297-300 (1995).
Nelson R.M. et al. Determination of accuracy in Neonates for non-invasive blood pressure device using an improved algorithm. Blood Pressure Monitoring 7, 123-9 (2002).
PATENTS
US 5,704,362 Method for oscillometric blood pressure determination employing curve fitting
US 5,579,776 Oscillometric blood pressure monitor with enhanced cuff pressure control
US 6,358,213 Calculation of quality and its use in determination of indirect noninvasive blood pressure
US 6,423,010 Oscillometric blood pressure monitor with improved performance in the presence of arrhythmias
US 6,746,403 Physiological-signal-analysis device for measuring a blood pressure and method
US 7,074,192 Method and apparatus for measuring blood pressure using relaxed matching criteria
US 7,070,566 Artifact rejection using pulse quality values
US 6,893,403 Oscillometric determination of blood pressure
US 5,680,870 Oscillometric blood pressure monitor which acquires blood pressure signals from composite arterial pulse signal