
Mechanical ventilation is a common supportive treatment utilized in the care of critically ill patients using fixed parameters. Yet, because patient breathing patterns are variable during ventilation, these fixed parameters may fail to deliver a mechanical breath that adapts to this variability in a patient’s ventilator demand and respiratory mechanics1. When this happens patient-ventilator asynchronies (PVAs) may occur, increasing the risk of poor outcomes2.
Ventilatory over-assistance or under-assistance results in a variety of asynchronies, each leading to different deleterious effects on patients. While over-assistance may lead to a lower patient inspiratory drive and result in reverse triggering and increased lung injury, under-assistance can increase the load on respiratory muscles and result in air hunger or lung injury due to excessive tidal volumes2.
Because of these varying clinical implications, and the dangers they represent to patients, identifying the type of asynchrony, as well as the causes behind it, is critical to providing safe and effective treatment for mechanically ventilated patients.
In this article, we’ll review the most common forms of asynchronies. We’ll also take a look at the clinical issues seen in each and the treatment options recommended to help reduce the risk of lung injury and enhance outcomes.
What is Patient Ventilator Asynchrony (PVA)?
Ideally, the strategy for mechanical ventilation in critically ill patients is to allow the patient to generate spontaneous breaths as quickly and safely as possible in order to reduce the risk of diaphragmatic dysfunction1.During spontaneous breathing, synchronous interaction between the patient and the ventilator must be maintained to reduce inspiratory effort while altering the ventilation setting based upon variation in breathing mechanics and ventilator demand1.
During spontaneous breathing, the pressure applied to the respiratory system is dependent upon the sum of the pressure generated by the respiratory muscles and that generated by the ventilator. This coordination is dependent upon numerous factors, including the patient’s pathophysiology, the patient-ventilator interface and ventilator settings utilized2.
Unfortunately, optimizing this patient ventilator interaction is challenging, and asynchronies occur when ventilator assistance fails to match the patient’s demand. Therefore, asynchronies can be thought of as poor patient-ventilator interaction or a lack of coordination between patient and ventilator caused by a mismatch between the magnitude of support demanded versus provided1,2.
Types of Asynchronies
As we discussed, asynchronies occur due to a mismatch between the technological variable involved in ventilator functioning and patient physiologic variables1. PVAs may be classified based on the phase of the respiratory cycle in which they occur2. This classification has also been revised depending on the extent of disturbance of coordination, either major or minor3.
Major PVAs include ineffective triggering, auto-triggering and double-triggering3. Minor PVAs include pre-mature or anticipated cycling, prolonged or delayed cycling and triggering delay. The most frequent PVAs are due to ineffective triggering, followed by double cycling2,3.
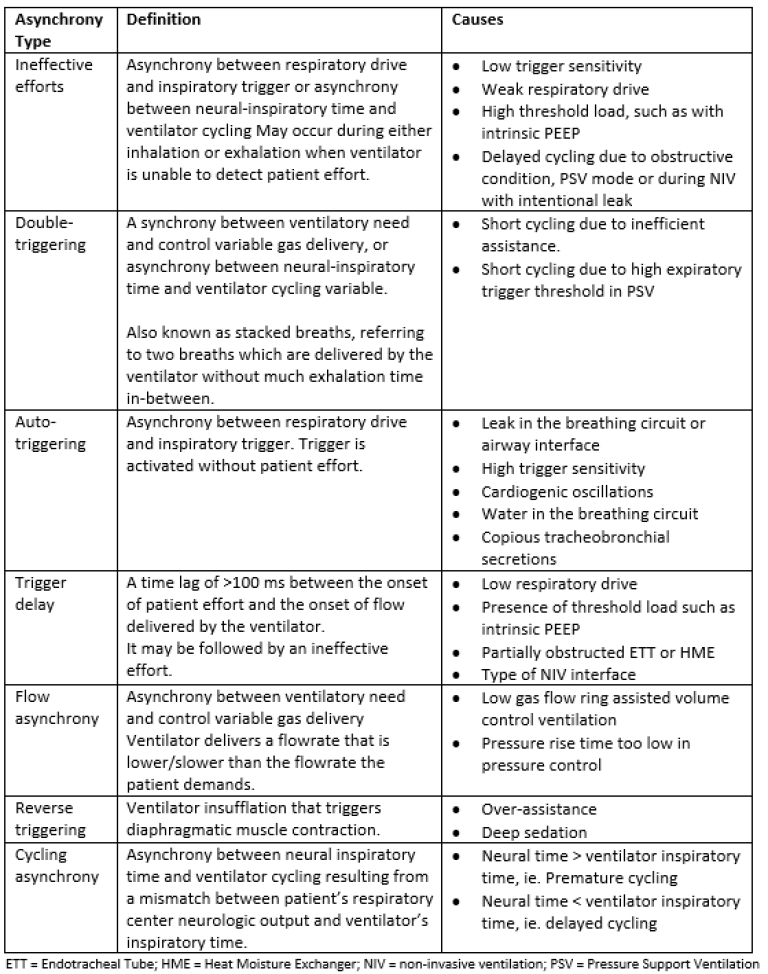
The following chart summarizes the most common asynchronies based on the work of Mirabella et al1:
Clinical Implications of Asynchrony
When patients are mechanically ventilated, it is crucial that the ventilator respond to patient effort. If the ventilator does not respond and an asynchrony occurs, weaning may become more difficult, leading to prolonged mechanical ventilation and increasing the risk of poor outcomes1,2.
Mechanical ventilation and asynchronies may also have a negative effect on hemodynamics. Should intrathoracic pressure increase due to double cycling, ventricular preload and afterload of ventricles is altered, thereby affecting cardiac output and hemodynamic status2. On the other hand, ineffective efforts can decrease intrathoracic pressure. Therefore, both asynchronies may lower the predictive accuracy of some hemodynamic parameters of fluid responsiveness2.
Additionally, there may be psychological risks involved with a PVA. Patients requiring mechanical ventilation already suffer from anxiety, fear and discomfort, all of which may be worsened due to an asynchrony2.
Research by Yoshida et al. also linked reverse triggering to worsening of pre-existing lung injury through a pendelluft effect from non-dependent lung areas toward dependent areas due to poor transmission of the diaphragm contraction across the pleural surface in an injured lung2.
The issue of lung injury has also been raised in researched focusing on double cycling. De Haro et al. found that the volume of stacked breaths that results from the inspiratory airflow mismatch can double the set tidal volume, exceeding the optimum set value for protective ventilation and potentially harming lung tissue and respiratory muscles2.
Overall, asynchronies have been associated with a worse prognosis, including2:
- Sleep disorders
- Discomfort
- Increased need for sedatives
- Prolongation of mechanical ventilation
- Increased intensive care unit (ICU) and hospital stays
- Increased mortality
Thus, appropriate monitoring and management of asynchronies plays a crucial role in improving patient-ventilator interaction, as well as patient care and safety.
Management of Asynchronies
Different strategies can be used to reduce the incidence of PVA during ventilation. Marta and Savino recommend the following strategies3:
- Avoid over-assistance, increasing patient respiratory drive by diminishing the inspiratory pressure support in order to decrease the rate of ineffective triggering.
- Reduce tidal volume and minute ventilation (particularly in COPD patients) to minimize PEEP and reduce the risk of ineffective triggering.
- Optimize inspiratory trigger sensitivity to reduce auto-triggering.
- Avoid deep sedation and long-lasting sedative drugs.
- Choose the correct NIV interface to avoid air leaks.
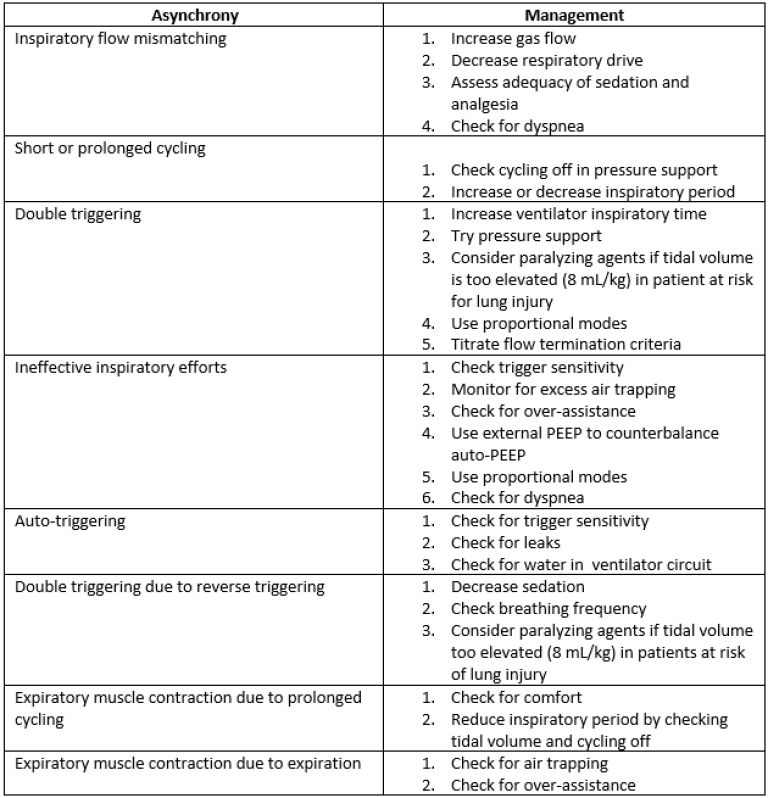
The following chart summarizes management options that may be employed in the case of a PVA4:
Summary
- Synchronous interaction between patient and ventilator must be maintained in order to provide optimal patient care.
- Because patient breathing patterns are variable, ventilation using fixed parameters may result in asynchrony.
- Risks of asynchrony include psychological problems, lung injury, and increased length of ICU and hospital stay and mortality.
- The most common PVAs are ineffective efforts and double cycling.
- Recognizing PVA early and employing effective management strategies may help improve patient care and safety.
Sources:
1: Mirabella, Lucia et al. “Patient-Ventilator Asynchronies: Clinical Implications and Practical Solutions.” Respiratory care vol. 65,11 (2020): 1751-1766. doi:10.4187/respcare.07284
2: de Haroet al. “Patient-ventilator asynchronies during mechanical ventilation: current knowledge and research priorities.” Intensive Care Medicine Experimental (2019),7 (Suppl1):43. https://doi.org/10.1186/s40635-019-0234-5
3: Lazerri, Marta and Savino, Spadaro. Teaching Pearls in Noninvasive Mechanical Ventilation Key Practical Insights. Chapter 18. Edited by Antonio M. Esquinas, Springer, 2022.
4: Esperanza, José Aquino et al. “Monitoring Asynchrony During Invasive Mechanical Ventilation.” Respiratory care vol. 65,6 (2020): 847-869. doi:10.4187/respcare.07404
© 2022 General Electric Company – All rights reserved.
GE and the GE Monogram are trademarks of GE. Reproduction in any form is forbidden without prior written permission from GE. Nothing in this material should be used to diagnose or treat any disease or condition. Readers must consult a healthcare professional.
JB21405XX
Lung Protective Ventilation in ARDS Patients
Listen to Professor Salvatore M. Maggiore, M.D., Ph.D. present a lecture series on how to implement lung protective ventilation strategies during mechanical ventilation of patients suffering from Acute Respiratory Distress Syndrome (ARDS) in the ICU.







