The Principles of Alarms
Managing a patient in an acute care setting not only involves establishing a proper diagnosis and treatment plan, it is imperative that the condition of the patient is assessed throughout this journey. Central to that is the introduction of patient alarms which are a means to alert a clinician when physiology deviates from normal. A simplistic view is that an alarm should trigger for bradycardia, when the heart rate is less than 50 beats per minute or for tachycardia when the heart rate is above 90 bpm.
The fundamental aspect of alarms is to serve as an early detection of patient deterioration, so that timely interventions can be deployed to prevent the patient from becoming critically ill. The other aspect of alarms is to alert clinicians when a device malfunctions, such as a disconnected sensor, or a disconnected breathing circuit for a patient being mechanically ventilated.
Stress and the burden of alarms
While alarms are an essential patient safety solution during patient management in the acute care setting, there are noted tradeoffs which include the burden of alarm fatigue. Simply stated, alarm fatigue results from a disproportionate number and frequency of alarms that are not clinically relevant or actionable, that results in careworkers becoming desensitized to them. In one study, only 5% to 13% of alarms were found to require some form of medical intervention.
In a study conducted by Schmid, they noted that 81% of all clinically irrelevant alarms to be the result of mild and/or brief violations in an alarm threshold. When implementing a threshold delay, the frequency of clinically irrelevant alarms dropped to 53.85%, while the positive predictive value increased from 28.16% to 46.15%.
This study is one example where alarm optimization can be realized, through adjustments in the duration of threshold violations.
At the extreme, alarm fatigue is a patient safety issue where life-threatening alarms may be missed due to sensory overload by the clinicians. The Joint Commission has recognized these patient safety concerns and has issued a warning to that effect. An effort to optimize the robustness of alarms saw the evolution into the multiparameter notification sets and the advent of early warning scores.
Additional alarm optimization strategies include the revision of thresholds, auto-adjustable thresholds that are based on patient normalized data, algorithms and artificial intelligence solutions such as neural networks and machine learning all have future potential. While some of these solutions may provide a technicological breakthrough, there comes one word of caution - clinicians often view “black box” algorithms with skepticism for they are viewed as “harder to interpret.” In the interim, there are opportunities to continue to advance alarm management and one area that warrants exploration is multiparameter notifications. This type of notification can take a series of parameters (e.g. heart rate, respiratory rate, SpO2 , etc.) and notify the clinician when all pre-defined criteria are met. This approach allows clinicians to customize individual alarm thresholds to more critical levels, while providing a multiparameter notification layer that triggers when a combination of lower-level threshold breaches are met.
The case for multi-parameter notifications and early warning scores
As early as the late 1990s an Early Warning Score (EWS) was developed with the aim to leverage multiparameter notification in an effort to identify patients at risk for early deterioration, that may require ICU transfer. While variations upon the original construct of the original EWS have emerged, the driving inputs remain - physiology variables including respiratory rate, oxygen saturation, temperature, blood pressure, heart rate and cognition. The clinical validity of these EWS has been demonstrated in both surgical and medically ill patients. Some of the EWS measures require manual entry, like urine output or Glasgow Coma Score, and this may introduce errors in measurement. To that effect, a UK study demonstrated that 38% of the early warning scores were either not entered completely or the calculation was incorrect, resulting in many cases of missed alerts. The introduction of automated EWS solutions reflect an example of how multiparameter notifications can be implemented leveraging an established clinical scoring tool.
Utilization of automated EWS have shown improvements in patient outcomes, including hospital survival, and hospital length of stay. There have been efforts beyond EWS development to further optimize the clinical robustness of alarms, and multiparameter notification continues to evolve. The demand for these notifications will continue to grow as more patients within the hospital will be providing continuous streams of vital signs and other physiologic measures where the burden of alarm fatigue is likely to intensify.
Other multiparameter notifications that have shown clinical utility are in the management of sepsis. As far back as the early 1990s Roger Bone introduced the concepts of SIRS or the systemic inflammatory response syndrome which reflects abnormalities in heart rate, temperature, respiratory and white blood cell count. Bedside monitoring can be leveraged to identify three of the four SIRS criteria and can form the foundation of multiparameter notifications for patients at risk for the development of sepsis. This highlights a challenge with predictive algorithms including multiparameter notifications - we frequently seek a one size fits all approach. Where, in fact, a more tailored approach based on disease state or clinical outcome may be more pragmatic.
Research has identified that there may be multiple sepsis phenotypes with Seymour documenting four. In their study, the alpha phenotype was the most prevalent and was associated with the lowest requirement of vasopressors and the lowest mortality rate (5%); this is contrasted to the delta phenotype that had the highest mortality rates of approximately 40%. In addition, most predictive alarms use a binary endpoint such as the need for ICU transfer, when in fact there are multiple pathways that result in deterioration and each have distinct signatures of illness. This was illustrated by Blackwell who identified that the four most common reasons for clinical deterioration requiring transfer to the ICU are: respiratory instability, infection and suspected sepsis, and heart failure. Furthermore, in their analysis, they identified that statistical models trained for individual clinical events were more informative. A similar conclusion was made by van Rossum wherein “alarm strategies for ward patients should focus on less severe events that are more common and inform the early phase of serious sequelae” where medical interventions may be more effective in reversing the deterioration cascade.
Where to go next? Potential applications for multiparameter notifications
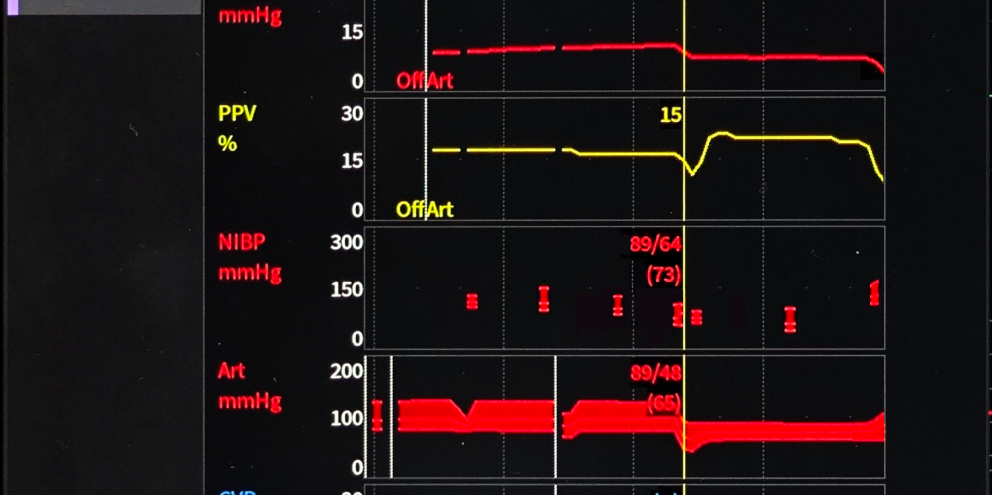
The use of multiparameter notifications that combine patient vitals signs along with other data streams, such as the patient monitor (electrocardiogram, hemodynamic parameters, etc.), mechanical ventilator or anesthesia delivery machine have yet to be explored. The potential to augment clinical decision making remains untapped but is worthy of exploration.
For instance, building upon SIRS criteria, multiparameter notifications could include altered mental status through use of sedation monitoring like entropy or the bispectral index. In addition, evaluating the impact of heart rate and respiratory rate variability that exists over a yet to be defined duration may provide an opportunity to further improve upon sepsis identification is worthy of consideration.
According to Vincent, respiratory compromise is one of the most common reasons for ICU admission from the hospital wards. A contributing factor for respiratory compromise stems from the use of opiates during the postoperative period. In fact the Emergency Care Research Institute has stated that inadequate monitoring of respiratory depression in patients receiving opioids is one of the top ten patient safety concerns facing hospitals. Respiratory depression can be identified via a suite of parameters that include: hypoxia via SpO2 , respiratory depression, and hypercapnia with end-tidal cooximetry. Additional parameters could offer utility in the development of multiparameter notifications which include the evaluation of adequacy of analgesia and depth of sedation.
Oversedation raises similar concerns that may impact hemodynamics. Therefore, the assessment of low or deep sedation levels in the face of hypotension, diminished systemic vascular resistance or low heart rate variability may be of clinical utility in the ICU. Addition of the minimum alveolar concentration can add relevance within the operating theatre.
A final area of consideration is during mechanical ventilation. The use of spontaneous breathing trials to support weaning affords the clinician with an assessment of patient readiness for extubation. However, during these trials, patient decompensation may occur and if unrecognized, pose risks to the patient as well as potentially delaying the time to extubation. The use of pulse oximetry, end-tidal co-oximetry, heart rate, respiratory rate and respiratory rate variability are simply a starting off point wherein multiparameter notifications can be developed.
Another opportunity for exploration is with regards to lung injury or worsening lung compliance that manifest from the development of acute respiratory distress syndrome (ARDS) or propagation of infection with SARS-CoV2. Monitoring compliance from the mechanical ventilator along with peak airway pressures, peak end-expiratory pressure, plateau pressures, pulse oximetry and PaO2 :FiO2 ratios has the potential to alert clinicians to the need for implementing or augmenting protective lung strategies.
In closing, the clinical utility of patient alarms is well established, but the burden of non-clinically actionable alarms that contribute to alarm fatigue continues to be a persistent source for concern. The implementation of multiparameter notification alerts with or without time delays may be the next step to alleviate some of this concern. It is notable to state that the clinical utility of these notifications may be dependent upon the endpoint selected, wherein hospital cardiac arrest or ICU transfer are routinely used. The challenge is that some of these events are infrequent. For example, in-hospital mortality occurs in 1-2% of patients while whereas one-year post-discharge mortality is more common (10%) and thus provides greater signal strength in order to establish relationships between clinical measures and risk. The development of multiparameter notifications will likely open the door for machine learning in order to identify the parameters and the meaningful thresholds that are associated with the outcome of interest, whether that is ICU transfer, 30 days readmission or others.
With simple visual cues by the multiparameter notifications, it can be used as a supplement to the alarms that attract strong visual and audible attention, allowing users to optimize the delay and threshold of the alarm to a value that provides greater signal strength of clinical risk. In other words, multiparameter notifications may function as an early warning to establish a buffer zone between "normal" and "critical", unlike the "one-size-fits-all" model of conventional alarm systems, thus offering the potential relief to users from alarm fatigue.