Introduction
Alarm management strategies that incorporate training, best clinical practices and sophisticated technology may help reduce alarm fatigue, improve clinician effectiveness and help enhance patient safety in hospital environments.
From 2005 to 2010, some 216 U.S. hospital patients died in incidents related to management of monitor alarms. This was determined from an analysis of the FDA database of adverse events involving medical devices, performed by the Boston Globe newspaper with help from ECRI Institute.¹
And ECRI Institute went further, stating that the actual number of such cases is “likely to be much higher,” since “most hospitals significantly underreport device-related incidents.”²
No one questions the importance of monitoring alarms in delivering quality care and protecting patient safety. Alarms alert clinicians to specific changes in patients’ condition and enable them to respond quickly and effectively. But too- frequent alarms that do not signal serious conditions can be a nuisance and cause stress for caregivers and patients in busy clinical areas.
Alarm fatigue may occur when the sheer number of monitor alarms overwhelms clinicians, possibly leading to alarms being disabled, silenced, or ignored.³
Healthcare providers were concerned about monitor alarms and alarm fatigue long before the issue came to national attention in February 2010. The Boston Globe reported on a patient who died at a major metropolitan hospital after the alarm on a heart monitor was inadvertently left off.⁴ Alarm hazards have been at or near the top of ECRI Institute’s list of “Top 10 Health Technology Hazards” since 2007, the first year the list was published,⁵ and ranked No. 1 for 2012.⁶
ECRI Institute reports that alarm-related adverse incidents typically involve staff becoming overwhelmed by the large volume of alarms, failure to restore alarms to their default or customized levels after they are modified to suit temporary conditions, and failure to relay alarms to ancillary notification systems such as pagers and wireless phones.⁷
The Spring 2011 issue of Horizons, a publication of the Association for the Advancement of Medical Instrumentation (AAMI), stated the problem succinctly: “When alarms work well, the environment of care is enhanced. When alarms don’t work well, they pull caregivers away from other duties and other patients–or worse, condition caregivers to ignore the alarm sounds altogether. Alarms that are ignored can and have resulted in patient deaths.”
The publication reported experts’ estimates that 85 to 99 percent of medical device alarms that sound do not require any action at the bedside, yet “add to the noise, confusion and stress in an already stressful environment.”⁷
The question is what to do. A review of recent literature suggests that the problem is complex and the solution multifaceted. Successful remedies can include a combination of:
- Realistic hospital-wide strategies to identify and address the underlying causes of alarm issues
- Thorough training of staff to understand how monitors function, how to set and respond to alarms
- Standardization of protocols for setting alarm levels
- Judicious, evidence-based adjustment of certain alarm limits to reduce false alarms
- Proper skin preparation and correct placement of ECG electrodes
- Customization of alarm settings according to patients’ condition
- Discontinuation of monitoring when no longer medically necessary
- More integration between monitoring parameters, so that alarms are more likely to signal clinically significant conditions, rather than temporary and harmless changes in one parameter
- Use of sophisticated monitor alarm technologies
Widespread concern
Patient monitors are only as reliable as the people who use them. Clinicians must understand monitoring systems and how to set alarm parameters appropriately to meet each patient’s needs. As early as 2002, The Joint Commission issued an alert on alarm safety and initiated a national patient safety goal to improve the efficacy of clinical alarms.⁹ Two years later, that goal was incorporated in The Joint Commission standards.
Still, alarm issues remain. An alarm safety web conference hosted by ECRI Institute addressed alarm fatigue and included a poll of attendees on alarm safety. When asked if they had experienced at least one serious clinical alarm event within the last two years, almost 75 percent of the 67 respondents said “yes.” Sixty-two percent rated the effectiveness of their hospitals’ alarm management programs as fair, and 9 percent rated it poor. None believed their program was excellent.¹⁰
One persistent issue is the sheer number of types of alarms and the diversity of devices. Many monitoring devices with alarms are used on a variety of patients with different medical conditions. Many also have multiple alarms. Two models of the same basic type of device may use different methods to set the alarms.
A 2006 white paper by the American College of Clinical Engineering found that caregivers had difficulty discerning six different alarm signals. For example, they might confuse an oxygen saturation alarm with a heart rate alarm, and as a result, miss a serious airway problem.¹¹ In other cases, caregivers may have trouble identifying the clinical situation associated with the alarm or defining how serious the situation is.¹²
Alarm limits are adjustable to serve patients of different ages and medical conditions, but this flexibility can be dangerous if misused. ECRI Institute reports many examples of alarm setting inappropriate to the patient type or care area. Some hospitals have not set specific alarm-setting protocols, and in those that have, staff may not always understand or follow them. Cases have been observed where two monitors of the same model were being used on patients with similar conditions, in the same care area, with completely different alarm settings.¹³
When confronted with multiple alarms, caregivers can become desensitized to them and may miss significant clinical events. A 2006 survey by the American College of Clinical Engineering covering more than 1,300 healthcare professionals showed that large percentages of respondents believed “nuisance” alarms occurred frequently (81 percent), disrupted patient care (77 percent), and can reduce trust in alarms, leading clinicians to disable them (78 percent).¹⁴
Alarm fatigue can be triggered by alarms that merely indicate clinically insignificant conditions that require no action from caregivers, according to an article in the Spring 2011 Horizons (AAMI): “Over time, these alarms are ignored by clinicians who are really looking for clinically significant true positives.”¹⁵
One study recorded tens of thousands of alarms in 30 days. In one critical care unit, a total of 39,000 alarms were recorded, averaging 1,300 alarms per day, or one alarm sounding every 66 seconds. In another critical care unit, the study observed approximately 600 alarms per patient per day.¹⁶
A study in a 15-bed medical progressive care unit at Johns Hopkins Hospital collected alarm data in December 2006 and January 2007. “During an 18-day period, the number of alarms totaled 16,953, equating to 942 alarms per day, or one critical alarm (crisis alarm, warning alarm, or system warning alarm) every 92 seconds.”¹⁷
In another study in a general care setting, nurses were asked how many alarms they could tolerate without alarm fatigue. They responded: Two to four alarms per patient per day.¹⁸
Not to be ignored is the effect of alarms and alarm mismanagement on patients and their families. The sound of an alarm from a bedside monitor adds anxiety to an already stressful situation.
“Alarms are disconcerting to patients and their families,” observed Mary Wyckoff, an acute care nurse practitioner in the Surgical Intensive Care Unit at Jackson Memorial Hospital in Miami, Fla. “When they hear an alarm go off, they assume something is wrong…allowing an alarm to continue to sound without resolving the situation is not only dangerous, but may seem dehumanizing to the patient.”¹⁹
Toward solutions
Hospitals have taken a variety of approaches to improve alarm management and address alarm fatigue. ECRI Institute recommends a disciplined, six-step strategic approach to improving monitor alarm safety. It includes:
- Assembling a multi-disciplinary team to work the issue
- Reviewing recent alarm-related events and near misses
- Observing alarm coverage processes and asking nurses and staff about their concerns
- Reviewing the entire alarm coverage system
- Identifying patient safety vulnerabilities and potential failures
- Developing realistic, implementable strategies to address underlying causes
On a more basic level, individual hospitals have followed highly specific and effective steps toward minimizing false alarms. One strategy is to reduce clinically meaningless alarms by judiciously making alarm thresholds less stringent. At Johns Hopkins Hospital, for example, a Comprehensive Unit Safety Program (CUSP) team led a project in the medical progressive care unit that reduced critical monitor alarms by 43 percent from baseline data (reported above), mainly by adjusting alarm defaults, carefully assessing and customizing monitor alarm parameters and limit levels, and enacting an interdisciplinary monitor policy. Specifically, the team:
- Widened the acceptable high and low heart rate levels, because patients were often undergoing physical therapy or got into and out of bed, resulting in large heart rate variations during the day
- Slightly lowered the default alarm setting for oxygen saturation because that parameter varied with activities such as ambulation and positioning
- Increased the premature ventricular contraction limit from 6 to 10 per minute to reduce alarms caused by benign premature atrial, junctional and ventricular beats.
As a result, the total number of alarms decreased from 16,953 during the baseline period studied to 9,647²⁰
Another study involving SpO₂ monitoring found that a time delay between detection of a low-saturation event and an alarm was highly effective in reducing alarm frequency. This technique works because the vast majority of desaturations below 90 percent self-correct in a short time. The study found that a 15-second alarm delay reduced alarm frequency by 70 percent.
A lower SpO₂ alarm threshold had similar effects. Here, lowering the alarm threshold from 90 percent to 88 percent reduced alarms by 45 percent, and lowering it to 85 percent reduced alarms by 75 percent. Combining delays and lower thresholds had even more impact: An alarm threshold of 88 percent with a 15-second delay reduced alarms by more than 85 percent.²¹
Alarm distribution is another way to mitigate alarm fatigue. Here, alarms are received in a central station and delivered to clinicians through wireless devices instead of sounding in the patient rooms. One concern with this model is that busy clinicians may not consistently “close the loop” by acknowledging the alarm, leaving the possibility that it has gone unheeded.
Beaumont Hospital successfully tested an alternate method, outfitting nurses with two-way communications badges in place of pagers. The study found that the badges significantly shortened time to first contact, time to completion, and rate of closure of the communication loop. Specifically, median time to first contact with the badges was 0.5 minutes, versus 1.6 minutes with pagers. The communication loop was closed in 100 percent of clinical alarms using badges versus 19 percent with pagers.²²
Impact of training
Effective protocol and education can have an impact on alarm frequency. Boston Medical Center, seeing a wide disparity in how staff members set alarm limits and experiencing numerous low-level alarms in its telemetry wards, enacted a program to standardize the alarm setting defaults in that care area. The hospital also created a telemetry training course for nurses and interns to reinforce alarm setting standardization. As a result, nuisance alarms were reduced.²³
The Johns Hopkins project determined that even with proper tailoring of alarms, crisis alarms could occur falsely, in large part because of poor skin preparation, poor electrode interface, patient movement and lack of adherence of electrodes. The team developed a checklist for alarm management competency that is now used to educate all new nurses. It includes information about electrode preparation, monitor skills, and troubleshooting.²⁴
In SpO₂ measurement, meanwhile, proper sensor application is critical, as an improperly applied sensor can result in a weak signal or light interference. There are many sensor configurations on the market, validated for specific applications, and biomedical personnel should know that using sensors outside their instructions for use may affect accuracy.
In addition, cables have a finite life, most notably in heavy-use areas like emergency departments and operating rooms. Cables nearing end-of-life can be a major cause of false alarms. Cables and cable connectors (also subject to mechanical stress and intermittent failure) should be inspected routinely and replaced on schedules to fit the care area.²⁵
Looking to technology
Technology is part of the solution for controlling false alarms and alarm fatigue. Ultimately, in the view of many experts, alarm technology should address how patients are doing from a holistic viewpoint–considering, for example, the relationships between pulse rate from various sources as well as oxygen saturation.
In this vision, “intelligent” alarms would integrate a variety of patient parameters and warn of serious changes in the patient’s overall condition. Such systems would not alarm for an individual outlier condition if other parameters were within the alarm settings–the outlier conditions would automatically be classified as not clinically significant. On the other hand, at times such alarms could sound earlier than on today’s discrete devices–such as if two or more parameters were trending in a wrong direction.²⁶
Meanwhile, monitor technologies already available are helping to enhance alarm accuracy and minimize false alarms.
Multi-lead algorithms
One important advance is multi-lead monitoring for arrhythmia, which analyzes data from the inferior, anterior and lateral views of the heart. Technologies that analyze only one or two leads fail to meet an American Heart Association recommendation that “...monitors should be capable of simultaneously displaying and analyzing two and preferably three or more leads.”²⁷
The benefits of multi-lead monitoring include:
- Reliable detection of cardiac events that might otherwise go unnoticed
- Discrimination of noise and artifact from true beats, reducing false alarms
- Multi-lead ST-segment analysis for assessment of myocardial ischemia
- Assurance of uninterrupted monitoring, even in case of an electrode contact failure
One multi-lead arrhythmia algorithm undergoes testing for each new version. The table below represents results from testing on common alarms from more than 2,000 hours on 114 telemetry patients.
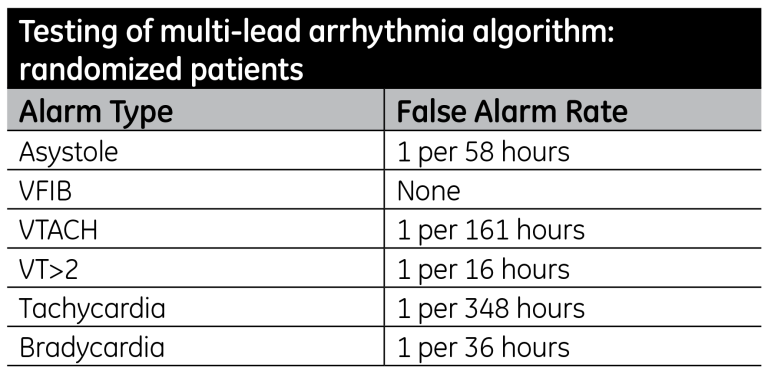
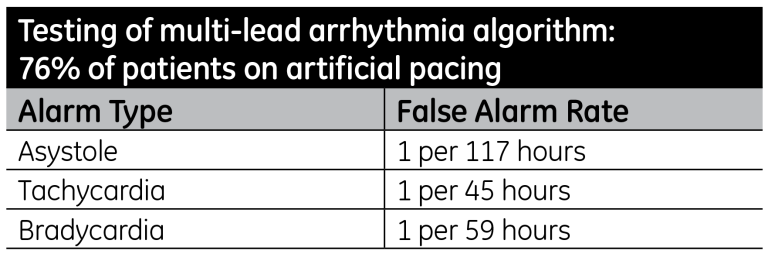
This latest version of this algorithm has shown significant improvement in heart rate accuracy and reduced false alarms compared to previous versions of the algorithm; specifically on patients with pacemakers, which often cause large errors in heart rates by introducing artifacts to the ECG waveforms. The algorithm was tested on more than 2,000 hours of ECG data from 100 randomized patients, of whom 76 had artificial pacing. (See Table 2).
The algorithm uses several advanced processing techniques:
- Continuous correlation, which compares the incoming multi-lead waveforms to beat “templates” as part of the QRS detection process, improving beat detection and recognition despite noise or artifact
- Incremental template updating, in which the multi-lead waveform templates used for beat classification and measurement accurately track subtle, progressive changes in beat shapes
- Contextual analysis, which uses information gained from neighboring beats in identifying arrhythmia events–evaluating features and information about the rhythm in a manner much similar to that used by a clinician
The algorithm is configurable for neonatal and pediatric patients to adapt for their unique waveform features.²⁸
Smart lead fail
Another innovation that helps reduce alarm volume is smart lead fail. This algorithm for multi-lead arrhythmia monitoring systems allows monitoring to continue without an audible alarm even if one lead (other than the right lower lead) becomes disconnected. Essentially, the remaining leads continue monitoring the heartbeat while the monitor displays an alert that a lead is off. Thus, the patient is safely monitored until a nurse can restore the lead connection. The system does sound a lead fail alarm if a second lead becomes disconnected.
Monitoring continues without the relearning process that takes place when a lead is lost in less sophisticated monitoring systems. In those cases, the patient is unmonitored for the few seconds it takes for the system to relearn the heart rhythm. Those delays can be hazardous in patients with life-threatening arrhythmias.
Telemetry smart alarms
Historically, pausing and reactivating alarms when telemetry patients remove their transmitters (such as for bathing or physical therapy) has been a manual process: Patient care staff must alert the central monitoring station when the transmitter is taken off and when it is replaced.
Smart alarms add a measure of automation to the process that enhances patient safety. Suppose that a nurse requests the central station to pause a patient’s alarm for a therapy session–but the patient’s transporter is delayed for 10 minutes. Now the alarm is silenced while the patient waits–a potentially hazardous situation.
With smart alarming, the central station alarm automatically reactivates after five minutes of continual ECG tracing, so long as the electrodes are still attached to the patient’s chest. This means that in case of a delay, the patient is without an alarm for a maximum of five minutes.
In a second scenario, the patient’s central station alarm is silenced for therapy or some other event of indeterminate length. When the procedure is over and the clinician reattaches the electrodes, the alarm reactivates automatically–no one needs to manually turn the alarm back on, and a potential source of human error is removed.
User-configurable alarm settings
User-configurable alarms let caregivers adjust default settings to tailor alarm parameters for the patient. For example, care-givers can adjust blood pressure alarm settings for a patient with lower-than-average pressure. For a person with a normal pulse rate in the 40s, the heart rate alarm threshold could be adjusted from default range of, say, 50 to 150, thus preventing multiple false alarms. Conversely, limits could be tightened and the alarm priority raised to detect a particular intermittent arrhythmia. Once the patient is discharged, the alarm configuration returns to the default settings.
For telemetry patients, the technology also enables caregivers to restore the monitor’s default alarm settings at the touch of a button. For example, at the beginning of a shift, the nurse could easily request the central station to revert to the original settings as a baseline and reconfigure the alarms to appropri-ately reflect the patient's current condition. The result may be fewer alarms and a higher percentage of clinically significant alarms.
The software also includes different default levels so that the bedside caregiver can choose alarm settings to suit specific patient profiles, such as trauma or cardiac cases.
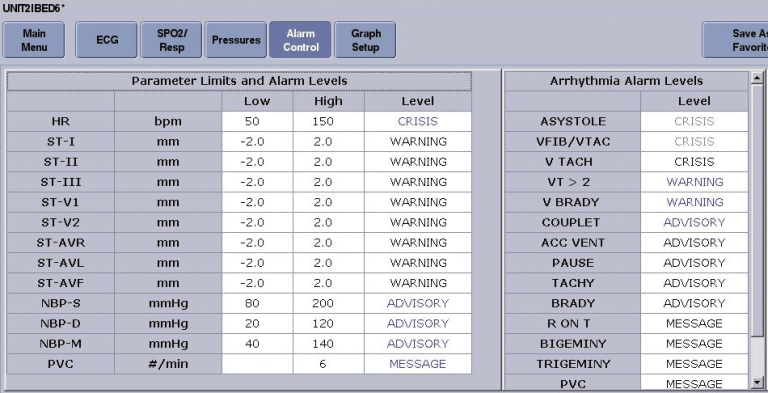
Absolute limits and locking limits
Absolute limits (guard limits) and locking limits provide checks against the potential misuse or erroneous use of alarm configurability. Absolute limits a nurse manager or a risk manager to fix the limits for a given parameter alarm to keep a caregiver from setting the high and low limits outside an acceptable range. It keeps alarm settings from being adjusted so wide that the alarm is essentially disabled. For example, an absolute limit might be set to ensure that the heart rate alarm cannot be set below 30 or above 160.
Locking limits allow facilities to ensure specific alarms are unable to be turned off under any circumstances. For example, a hospital may use locking limits to enforce a policy that all cardiac patients must have continuous life-threatening arrhythmia monitoring.
Escalating alarms
Escalating alarm technology automatically raises an alarm’s priority if a caregiver does not respond within a specified time. A parameter alarm may start at low priority and escalate to medium, then high. The escalation adds assurance that busy clinicians will be alerted to a persistent patient condition requiring attention.
Latching alarms
Latching allows alarms to be configured to continue sounding in case of intermittent but potentially life-threatening conditions, such as certain arrhythmias (asystole, ventricular tachycardia, ventricular fibrillation). Instead of the alarm shutting off when the event passes, it remains active until a caregiver acknowledges it.
SpO₂ monitoring
The latest advanced digital signal processing technologies for pulse oximetry monitoring help deliver accurate SpO₂ and pulse rate readings even in the face of challenging conditions such as patient motion and low perfusion–a potentially major source of false alarms.
Conclusion
Alarm safety and alarm fatigue are critical issues and solutions require a systems-level, multidisciplinary analysis of root cause. Effective alarm management initiatives are built on coordinated strategies that combine staff training, evidence-based procedures and protocols, and identification of best practice. Such efforts also include the use of appropriate monitoring and alarming technologies, tailorable to specific patient conditions. Effective alarm management can significantly help in enhancing patient safety and reducing caregiver stress in busy clinical environments.
References
- Kowalczyk, L. “Patient alarms often unheard, unheeded.” The Boston Globe (13 February 2010).
- Keller, J.P. “Making Clinical Alarm Management a Patient Safety Priority.” Tech Nation. ECRI Institute (April 2011).
- Graham, K.C. and Cvach, M. “Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms.” American Journal of Critical Care 19, No. 1, 28–34 (January 2010).
- Kowalczyk, L. “MGH death spurs review of patient Monitors.” The Boston Globe (21 February 2010).
- “Impact of clinical alarms on patient safety.” ACCE Healthcare Technology Foundation (2006).
- Keller, J.P. “Making Clinical Alarm Management a Patient Safety Priority.” Tech Nation. ECRI Institute (April 2011).
- Keller, J.P. “Making Clinical Alarm Management a Patient Safety Priority.” Tech Nation. ECRI Institute (April 2011).
- “Alarms Pose Challenges to Healthcare Facilities.” Horizons. Association for the Advancement of Medical Instrumentation (Spring 2011).
- “Impact of clinical alarms on patient safety.” American College of Clinical Engineering. [Online.] http://www.thehtf.org/White%20Paper.pdf.
- Keller, J.P. “Making Clinical Alarm Management a Patient Safety Priority.” Tech Nation. ECRI Institute (April 2011).
- “Impact of clinical alarms on patient safety.” American College of Clinical Engineering. [Online.] http://www.thehtf.org/White%20Paper.pdf.
- Phillips, J. and Barnsteiner, J. H. “Clinical alarms: improving efficiency and effectiveness.” Crit Care Nurs Q. 28 (4), 317–323 (2005). [Online.] www.ncbi.nlm.nih.gov/pubmed/16239820. Accessed 25 October 2009.
- Keller, J.P., et al. “Why Clinical Alarms are a ‘Top Ten’ Hazard: How you can help reduce the risk.” Horizons, Association for the Advancement of Medical Instrumentation (Spring 2011).
- Drew, B.J., et al. “Practice standards for electrocardio-graphic monitoring in hospital settings.” American Heart Association Scientific Statement 110 (17), 2721–2746 (2004).
- Gross B., et al. “Physiologic monitoring alarm load on medical/surgical floors in a community hospital.” Horizons, Association for the Advancement of Medical Instrumentation (Spring 2011).
- Logan, M. (Moderator). “A roundtable discussion: Alarm safety: a collaborative effort.” Horizons, Association for the Advancement of Medical Instrumentation (Spring 2011).
- Graham, K.C. and Cvach, M. “Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms.” American Journal of Critical Care 19, No. 1, 28–34 (January 2010).
- Taenzer, A.H. et al. “Impact of Pulse Oximetry Surveillance on Rescue Events and Intensive Care Unit Transfers.” Anesthesiology 112, 282–7 (2010).
- Wyckoff, M. “Improving how we use and respond to clinical Alarms.” American Nurse Today 4 No 9, 37–39 (Nov/Dec 2009).
- Graham, K.C. and Cvach, M. “Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms.” American Journal of Critical Care 19, No. 1, 28–34 (January 2010).
- Welch, J. “An evidence-based approach to reduce nuisance alarms and alarm fatigue,” Horizons, Association for the Advancement of Medical Instrumentation (Spring 2011).
- Bonzheim, K., et al. “Original Research: Communication Strategies and Timeliness of Response to Life Critical Telemetry Alarms.” Telemedicine and e-Health 17, No. 4, 241–246 (May 2011).
- “ECRI Institute. Best Practices for Health Technology Management: Valuable Lessons from the 2010 Health Devices Achievement Award Finalists.” Health Devices 39 (12), 444–9 (December 2010).
- Graham, K.C. and Cvach, M. “Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms.” American Journal of Critical Care 19, No. 1, 28–34 (January 2010).
- Welch, J. “An evidence-based approach to reduce nuisance alarms and alarm fatigue,” Horizons, Association for the Advancement of Medical Instrumentation (Spring 2011).
- Keller, J.P., et al. “Why Clinical Alarms are a ‘Top Ten’ Hazard: How you can help reduce the risk.” Horizons, Association for the Advancement of Medical Instrumentation (Spring 2011).
- Mirvis, D.M., et al. “Instrumentation and practice standards for electrocardiographic monitoring in special care units. A report for health professionals by a Task Force of the Council on Clinical Cardiology.” American Heart Association 79, 464–471 (February 1989).
- The GE EK-Pro Arrhythmia Detection Algorithm for Patient Monitoring, ©2008 General Electric Company. DOC0461863







