Abstract
The past ten years in healthcare have witnessed a convergence of two significant movements that have prompted a revisiting of care delivery within the hospital, including the critical care environment. On one front, global demographic shifts have led to an increasingly older population, while at the same time the workforce is shrinking. Healthcare labor–including critical care nurses and physicians–are retiring at a faster rate than the education system is replenishing these losses. These severe challenges have been compounded by the dramatic impact of the COVID-19 pandemic. The healthcare industry must envision novel care delivery models to handle these converging crises. This article highlights the impacts of demographic challenges and COVID-19 on the healthcare system and introduces the concept of adaptable acuity. This framework can serve as a model for flexible care delivery to support future needs within the hospital, including pandemic responsiveness.
The numbers game
The population is aging globally, and statistics from Europe help to illustrate this point. Between 2019 and 2050, Eurostat projects that the population of very old people will more than double.1 A graphical depiction of the aging population is represented in a population pyramid from Eurostat. The population of people older than 85 years will grow from 12.5 million in 2019 to 26.8 million by 2050. What is even more striking is the growth of the centenarian population. In 2019, there were 96,600 centenarians, and this number is projected to increase to 484,000 by 2050. The challenge with the aging demographic is that comorbid conditions are positively correlated with age, which places increasing constraints on the healthcare system to deliver care.
According to the U.S. Centers for Medicare & Medicaid Services (CMS), one-third of U.S. health expenditures are the result of hospital-based care.2 Most hospitalizations come from the emergency department (ED).3 The demand for ED visits and hospitalizations have grown over the past 2 decades. In the United States, there was an 18.4% increase in ED utilization between 2006 and 2014, with the number of annual visits rising from 89.6 to 106 million.4 Admissions from the ED also grew by 8.4%, increasing from 17.4 to 18.6 million. Similarly, in the United Kingdom, ED admissions increased annually by 3.2% between 2008 and 2018.5 More concerning for the U.K. National Health Services (NHS) is that hospital bed space grew a mere 0.3% per year during this time frame. The NHS also reported a concurrent increase in the medical complexity of admitted patients during this time. The number of patients admitted from the ED with more than five comorbid conditions grew from one in ten (2006-7) to one in three (2015-16). Additionally, admissions for elderly patients over 85 years increased by nearly 60%. This data highlights the growing demands placed on hospitals in the U.K. as they strive to deliver care to an aging and more complex patient population, all while bed capacity remains relatively stagnant. The financial burdens are similarly noteworthy. The cost of emergency admissions reached £17 billion in 2016-17, an increase of £5.5 billion in ten years.
These demographic trends are even more concerning when looking at rural healthcare. Between 2005 and 2016, rural ED visit rates in the United States rose from 36.5 to 64.5 visits per 100 persons, which is a more than 50% increase and outpaces the growth in ED visit volumes in the urban centers.6 Several factors have contributed to this surge in rural ED demand, including lack of funding and a shortage of primary care physicians compounded by high turnover.
Lastly, the demographic crunch has also affected the ICU, where many acute-care hospitals lack adequate coverage by intensivists and critical care trained nurses. According to the World Health Organization, 48% of hospitals surveyed by the American Hospital Association before the pandemic reported critical care labor shortages.7 Since the onset of the COVID-19 pandemic, the labor problems in the ICU have only intensified.8
Organizational stressors: The COVID-19 pandemic
The pandemic was the accelerant that allowed the demographic and bed capacity constraints to turn into a major crisis. Hospitals became overwhelmed due to excessive demand, combined with inadequate bed space and staffing. In fact, early simulations predicted that ICU bed capacity would need to expand by multiples, further highlighting the crisis.9–11 In addition to the lack of beds, several factors made care delivery challenging, including a shortage of supplemental resources such as medical gas outlets and electrical capacity; poor patient visibility; and the challenge of separating COVID from non-COVID patients.
To illustrate the stress placed on the ICU, the standard ICU bed capacity in the U.S. was 4,931 before the pandemic and increased to 7,630 during the pandemic surge.12 Furthermore, in 66% of hospitals, ICU bed capacity was opened in non-ICU locations where care was administered by hybrid teams of ICU staff augmented by surge support staff. More concerning were the staffing ratios impacting nursing care. During the pandemic, the ratio of patients per ICU nurse increased from 2.0 to 1 to 2.4 to 1. Non-ICU nurses were employed in 85% of the participating ICUs evaluated. These surge capacity beds absorbed almost 40% of the ICU admissions with little difference in their underlying comorbidities, except for a higher likelihood of COPD and immunosuppression cases being admitted in a traditional ICU bed.
The COVID pandemic highlighted the vulnerabilities that hospitals had to face when the prioritization of the COVID-infected could defer attention of other medical conditions.13 Balancing the care needs of both COVID and non-COVID patients became paramount, which prompted the reconfiguration of service delivery within the hospital to ensure flexibility in terms of physical structure and facility resources.
One viable solution to these vulnerabilities is the concept of adaptable acuity. This new term refers to the ability for hospitals to manage their physical and personnel resources to provide care in a flexible, effective, and patient-centered manner. This approach minimizes patient transfers within the hospital by not moving the patient based on their acuity, but rather by moving resources and care to the patient. It is estimated that avoiding patient transfers can reduce the average hospital length of stay by at least 0.5 days.14 The adaptable acuity model may provide the flexibility required to support both current and future hospital needs, especially when future surges in demand arise.
Critical care delivery change: Adaptable acuity
In the aftermath of the COVID-19 pandemic, the Society for Critical Care Medicine (SCCM) stated that “the ideal ICU patient room would facilitate the provision of patient-centered care, access and visibility to the patient from outside, while allowing access to and control of devices remotely and minimizing non-direct patient care entry. At the same time, privacy and a quiet environment for the patient are important.”15 The SCCM mentioned that the use of adaptable acuity patient care has successfully improved the quality of care for cardiac patients. Simply stated, adaptable acuity implies that the environment changes to the patient’s needs rather than moving the patient based on their acuity.
To date, most of the studies evaluating the implementation of adaptable acuity models have focused on the cardiothoracic surgery care area.16–18 Experience from the University of Wisconsin demonstrated that this approach led to significant reductions in hospital length of stay and ICU readmission rates.16 The adaptable acuity concept has extended beyond cardiac surgery care to include thoracic surgery,19 oncology,20 and neurology, specifically stroke.21
The successful implementation of this model depends on the training and staffing of a flexible nursing team, as well as the support of technology enablers. During the pandemic, it is important to mention that healthcare workers experienced significant levels of mental stress. Burnout was already present prior to the pandemic and only intensified thereafter.22,23 The adaptable acuity model requires additional training of nursing staff who can support the flexing up and down of acuity. Furthermore, staffing models will need to adjust, as staffing assignments may need to change throughout the day. Tiered staffing models have been proposed to allow for both intensivist and ICU nurses to oversee non-ICU staff, expanding the scope of critical care services within the hospital.24
Technology enablers
The transition towards adaptable acuity care models will be augmented with the deployment of technology solutions to streamline gaps in care delivery; these solutions are referred to as technology enablers and are summarized in Table 1.
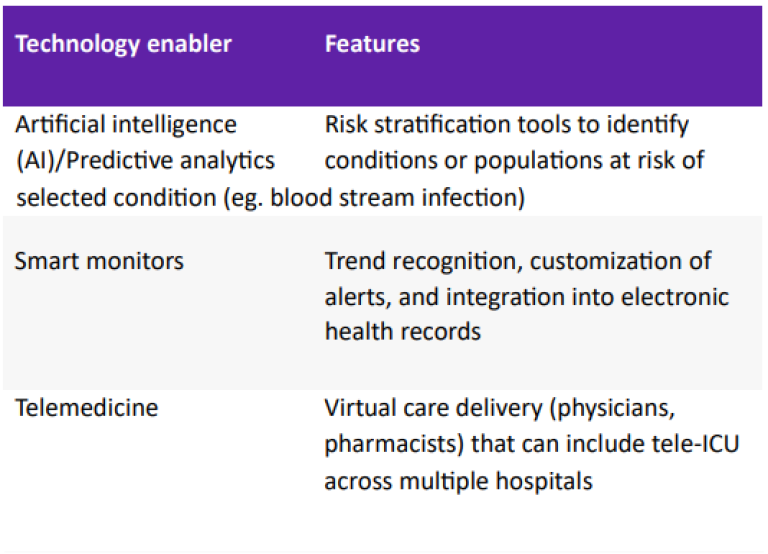
Technology enablers may include predictive algorithms, or what is commonly termed artificial intelligence (AI). These tools help clinicians stratify patients into risk pools, which enables a tiered response of care.25 These predictive algorithms can focus on minimizing alarms which require no clinical action and identify patients at risk of respiratory failure, cardiac arrest, or blood stream infections, to name a few. Other technology enablers include smart monitors and sensors that can further aid the clinician in receiving actionable information.26 Telemedicine has also been reported to improve care delivery in rural hospitals, where the ICU length of stay and mortality were reduced by 34% and 32% respectively following the first year of implementation.27 Tele-ICU expands the telemedicine concept further by providing a virtual command center that connects ICU staff across multiple units within a hospital or can expand to support multiple hospitals within a network.28 Studies have shown a reduction in mortality rates and ICU lengths of stay following implementation of tele-ICU.28
Organizational implementation
The need for organizational change and the development of adaptable acuity capabilities within a hospital are merely the first steps to implementing this model. Once stakeholders agree that this change is necessary, the next step involves mapping out the design and implementation plans. Brambilla et al. have conducted a thorough analysis of the facility assessment for flexible designs. Their study can serve as a starting point for designing future state solutions that are appropriate for each facility.29
Another important consideration is the deployment strategy for implementing an adaptable acuity delivery model. Given the limited published research available on this topic, perhaps it is best to pose a series of questions that can help align the organizational change process:
- What disease states will the model include?
- How will clinicians (nurses, physicians, respiratory therapists, and others) be trained to excel in a flexible acuity, flexible staffing environment?
- How can leaders ensure buy-in across the organization? Will this be a bottom-up, top-down, or hybrid adoption model?
- How will obstacles and successes be monitored in order to allow further refinement in the future?
- How can U.S. organizations manage the potential medico-legal issues that may arise when credentialed healthcare workers treat patients in care areas outside of their credentials?
- What safeguards will be implemented to minimize staff burnout and turnover?
The COVID pandemic highlighted existing vulnerabilities within the healthcare system that will continue to worsen given the demographic shifts from now through 2050. Models such as adaptable acuity may give hospitals the ability to provide flexibility in care delivery, especially during states of crisis like future pandemics. The roadmap for the design and implementation of adaptable acuity units has been largely based in the cardiac surgery care area. Thus, more investigation is needed to explore the implementation across broader care areas.
References
- European Commission. Statistical Office of the European Union. Ageing Europe: looking at the lives of older people in the EU: 2020 edition. [Internet]. LU: Publications Office; 2020 [cited 2023 Sep 16]. Available from: https://data.europa.eu/doi/10.2785/628105.
- NHE Fact Sheet | CMS [Internet]. [cited 2023 Sep 24]. Available from: https://www.cms.gov/data-research/statisticstrendsandreports/national-health-expenditure-data/nhe-factsheet.
- Gonzalez Morganti K, Bauhoff S, Blanchard JC, Abir M, Iyer N, Smith A, et al. The Evolving Role of Emergency Departments in the United States [Internet]. RAND Corporation; 2013 May [cited 2023 Sep 24]. Available from: https://www.rand.org/pubs/ research_reports/RR280.html.
- Lin MP, Baker O, Richardson LD, Schuur JD. Trends in Emergency Department Visits and Admission Rates Among US Acute Care Hospitals. JAMA Intern Med. 2018 Dec;178(12):1708–10.
- Emergency admissions in the NHS increase by almost half in a decade due to rise in sicker patients, new research shows [Internet]. [cited 2023 Sep 16]. Available from: https://www. health.org.uk/press-release/emergency-admissions-inthenhsincrease-by-almost-half-in-a-decade-due-to-rise-in.
- Greenwood-Ericksen MB, Kocher K. Trends in Emergency Department Use by Rural and Urban Populations in the United States. JAMA Network Open. 2019 Apr 12;2(4):e191919.
- Halpern NA, Pastores SM, Oropello JM, Kvetan V. Critical Care Medicine in the United States: Addressing the Intensivist Shortage and Image of the Specialty*. Critical Care Medicine. 2013 Dec;41(12):2754–61.
- Jatoi NN, Awan S, Abbasi M, Marufi MM, Ahmed M, Memon SF, et al. Intensivist and COVID-19 in the United States of America: a narrative review of clinical roles, current workforce, and future direction. Pan Afr Med J. 2022;41:210.
- Tonetti T, Grasselli G, Zanella A, Pizzilli G, Fumagalli R, Piva S, et al. Use of critical care resources during the first 2 weeks (February 24-March 8, 2020) of the Covid-19 outbreak in Italy. Ann Intensive Care. 2020 Oct 12;10(1):133.
- Moghadas SM, Shoukat A, Fitzpatrick MC, Wells CR, Sah P, Pandey A, et al. Projecting hospital utilization during the COVID19 outbreaks in the United States. Proc Natl Acad Sci U S A. 2020 Apr 21;117(16):9122–6.
- Grasselli G, Pesenti A, Cecconi M. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA. 2020 Apr 28;323(16):1545–6.
- Greco M, De Corte T, Ercole A, Antonelli M, Azoulay E, Citerio G, et al. Clinical and organizational factors associated with mortality during the peak of first COVID-19 wave: the global UNITE-COVID study. Intensive Care Med. 2022 Jun 1;48(6):690–705.
- Troisi R, De Simone S, Vargas M, Franco M. The other side of the crisis: organizational flexibility in balancing Covid-19 and nonCovid-19 health-care services. BMC Health Services Research. 2022 Aug 29;22(1):1096.
- 14. The Role of the Physical Environment in the Hospital of the 21st Century: A Once-in-a-Lifetime Opportunity | The Center for Health Design [Internet]. [cited 2023 Sep 29]. Available from: https:// www.healthdesign.org/knowledgerepository/rolephysicalenvironment-hospit…;
- Society of Critical Care Medicine (SCCM) [Internet]. [cited 2023 Sep 24]. SCCM | Configuring ICUs in the COVID-19 Era. Available from: https://sccm.org/COVID19RapidResources/Resources/ Configuring-ICUs-in-the-COVID-19-Era-A-Collection.
- Chindhy SA, Edwards NM, Rajamanickam V, Lushaj EB, Lozonschi L, De Oliveira NC, et al. Acuity adaptable patient care unit system shortens length of stay and improves outcomes in adult cardiac surgery: University of Wisconsin experience. Eur J Cardiothorac Surg. 2014 Jul;46(1):49–54.
- Clark EI, Roberts CL, Traylor KC. Cardiovascular Single-Unit Stay: A Case Study in Change. American Journal of Critical Care. 2004 Sep 1;13(5):406–9.
- Winter M, Tjiong L, Houston SL. The challenges and rewards of the cardiac universal bed model. Nursing Management. 2011 Jan;42(1):46.
- Hennon MW, Kothari A, Maloney JD, Weigel T. Implementation of an Acuity Adaptable Patient Care Unit is associated with improved outcomes after major pulmonary resections. J Surg Res. 2011 Sep;170(1):e17-21.
- Acuity Adaptable Nursing Units in Oncology - ProQuest [Internet]. [cited 2023 Sep 29]. Available from: https://www.proquest. com/openview/f1c562de56aee0e639d71b915c787cba/1?pqorig site=gscholar&cbl=37213.
- Alexandrov AW, Coleman KC, Palazzo P, Shahripour RB, Alexandrov AV. Direct stroke unit admission of intravenous tissue plasminogen activator: safety, clinical outcome, and hospital cost savings. Ther Adv Neurol Disord. 2016 Jul 1;9(4):304–9.
- Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity. 2020 Aug 1;88:901–7.
- Azoulay E, De Waele J, Ferrer R, Staudinger T, Borkowska M, Povoa P, et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Annals of Intensive Care. 2020 Aug 8;10(1):110.
- Aziz S, Arabi YM, Alhazzani W, Evans L, Citerio G, Fischkoff K, et al. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med. 2020;46(7):1303–25.
- Martin GS. Cover Story: The Future ICU., ICU Management & Practice, Volume 19 Issue 4, Winter 2019/2020
- Islam MdM, Rahaman A, Islam MdR. Development of Smart Healthcare Monitoring System in IoT Environment. SN COMPUT SCI. 2020 May 26;1(3):185.
- Modern Healthcare [Internet]. 2019 [cited 2023 Sep 29]. Telemedicine helps rural hospitals meet intensivist shortage. Available from: https://www.modernhealthcare.com/caredelivery/telemedicineh elps-rural-hospitals-meet-intensivistshortage.
- 28. Kumar S, Merchant S, Reynolds R. Tele-ICU: Efficacy and Cost Effectiveness Approach of Remotely Managing the Critical Care. Open Med Inform J. 2013 Aug 23;7:24–9.
- 29. Brambilla A, Sun TZ, Elshazly W, Ghazy A, Barach P, Lindahl G, et al. Flexibility during the COVID-19 Pandemic Response: Healthcare Facility Assessment Tools for Resilient Evaluation. Int J Environ Res Public Health. 2023 Oct 31; 18(21):11478
Data subject to change.
© 2023 GE HealthCare. GE is a trademark of General Electric Company used under trademark license. All other trademarks are property of their respective owners. Reproduction in any form is forbidden without prior written permission from GE HealthCare.
Nothing in this material should be used to diagnose or treat any disease or condition. Readers must consult a healthcare professional.
JB26869XX 11/2023

Prof. Maurizio Cecconi, MD FRCA FFICM MD(Res)
Chair of the Department of Anaesthesia and Intensive Care
IRCCS Istituto Clinico Humanitas
Professor of Anaesthesia and Intensive Care
Vice President MEDTEC School Humanitas University
Immediate Past President of the European Society of Intensive Care Medicine (ESICM)
Maurizio Cecconi is a full-time professor of Anaesthesia and Intensive Care at Humanitas Research Hospital and Humanitas University, Milan, Italy. Previously he worked as Reader and Clinical Director at the Adult Critical Care Department, St George’s Hospital and University of London, UK. Maurizio does research in Intensive Care Medicine, Anaesthesia, Perioperative Medicine, and Emergency Medicine.

Dr. Robert N. Bilkovski, MD, MBA
President, RNB Ventures Consulting Inc.
Dr. Bilkovski has broad management experience, having served in leadership roles in multiple Fortune 500 companies overseeing medical affairs and clinical development in IVD, medical device, and pharmaceuticals industries. Some of the companies where he served in leadership roles include Hospira, GE HealthCare, Abbott Laboratories, and Becton Dickinson. Robert currently is the President of RNB Ventures Consulting Inc. providing strategic consulting in the field of medical and clinical affairs for medical device and diagnostic companies.
Dr. Bilkovski received his undergraduate degree in biochemistry with a focus in genetic engineering at McMaster University in Hamilton, Ontario, Canada. Robert completed his medical training at Rosalind Franklin University/The Chicago Medical School and subsequently pursued specialization in emergency medicine. Lastly, Dr. Bilkovski earned his MBA at the University of Notre Dame as part of his transition from clinical medicine to medical industry.








