What is cardiac output and PiCCO®?
Cardiac output (C.O.) is the amount of blood ejected by the heart every minute to the peripheral circulation. The C.O. is the product of the heart rate (HR) times the stroke volume (SV), whereby the SV is the amount of blood ejected by the ventricle with every beat. Normally both ventricles pump the same amount of blood in a minute.
The primary function of the heart is to deliver sufficient oxygen and nutrients to the tissues. Under normal conditions C.O. varies in order to comply with the total tissue needs. These may change secondary to exercise, infection, heart disease, trauma, surgery or administration of drugs. Measured C.O. can be normalized to a patient’s body surface area (BSA) by dividing C.O. by the BSA. The resulting value is called cardiac index (CI).
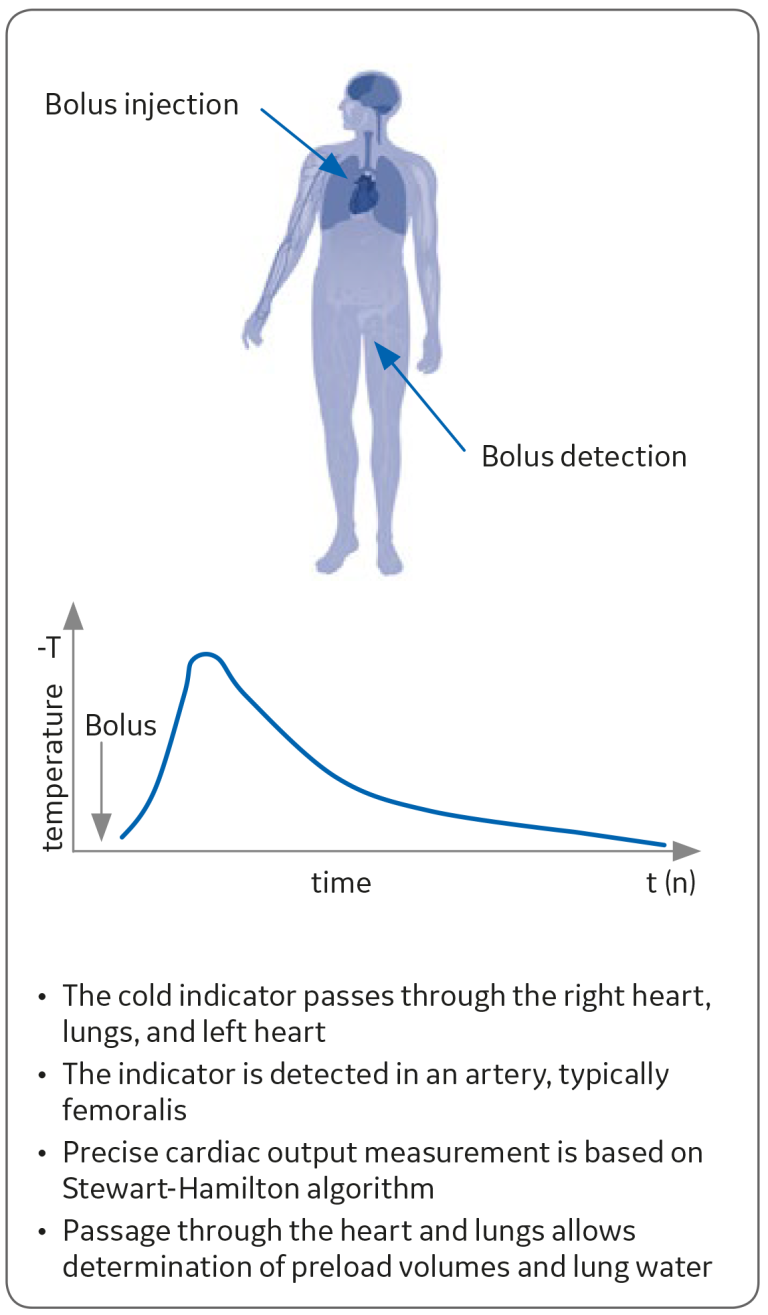
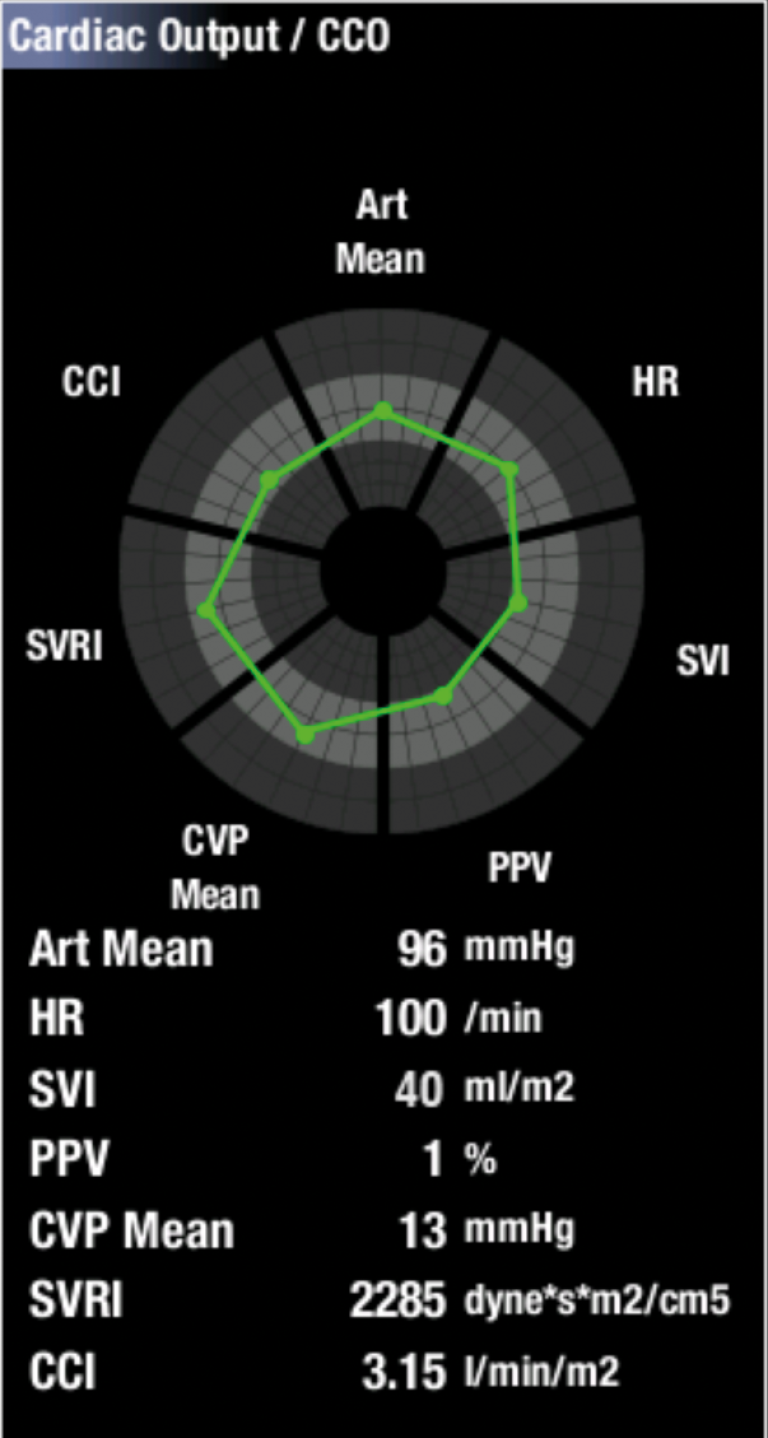
PiCCO continuous cardiac output (CCO) measures cardiac output continuously, and it does not require right heart catheterization (pulmonary artery catheter). The measurement is calibrated by transpulmonary thermodilution. see Figure 1.
While the essence of PiCCO monitoring is around cardiac output, it also measures parameters related to preload, afterload, and contractility, and extra vascular lung water. Therefore, it can provide a more comprehensive view on a patient’s hemodynamic status than just blood flow. Since PiCCO technology does not require right heart catheterization, it is less invasive than other technologies.
The use of PiCCO technology requires a standard central venous catheter for transpulmonary thermodilution and a specific PiCCO catheter, inserted in femoralis, radialis, brachialis, or axillary artery.
PiCCO has shown to be effective in terms of cost and information obtained for clinician’s decision making.¹
How PiCCO parameters are measured
Flow
Transpulmonary thermodilution is utilized for calibrating the continuous cardiac output calculation. A known amount of cold injectate at a known temperature is injected through the central venous catheter. After the injection, the change in blood temperature is measured near the tip of the PiCCO catheter in the artery. A curve of the temperature change over time is displayed in the C.O. View of the patient monitor. This is called a thermodilution curve, see Figure 1. C.O. is calculated by using the formula of Stewart-Hamilton from the average of the selected/approved thermodilution curves. Since the bolus passes through the heart and the lungs, preload and extra vascular lung water values can also be determined. The calibration is recommended once in eight hours, or after a significant change in the hemodynamic status (e.g. due to medication, fluid loading). Intracardiac shunts and valve insufficiencies may impact the accuracy of transpulmonary thermodilution. The same is true for any thermodilution technology.²
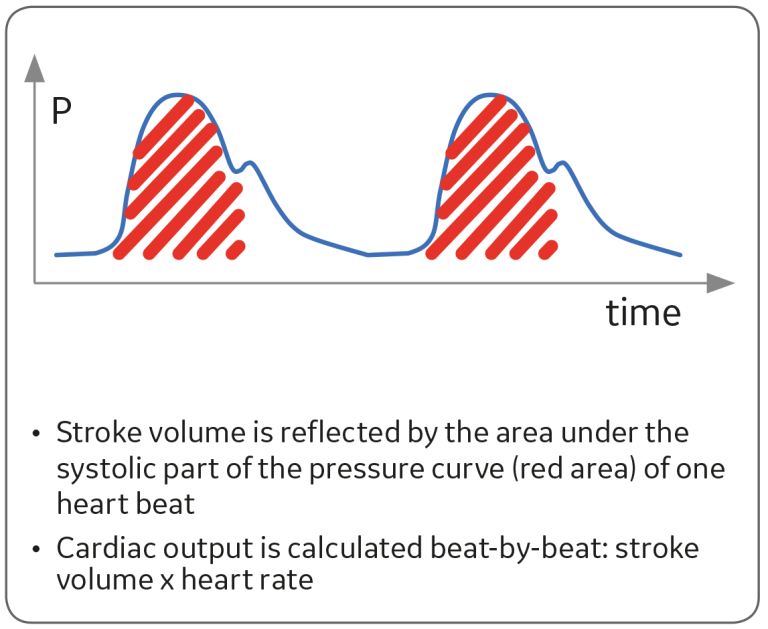
PiCCO continuous cardiac output monitoring is based on pulse contour analysis of the invasive arterial blood pressure curve. Stroke volume is calculated for each pulse using the pulse contour analysis. With this and heart rate, continuous cardiac output can be defined; see Figure 2. The indexed value is the same divided by the body surface area.

Factors affecting C.O. determination and calibration by transpulmonary thermodilution
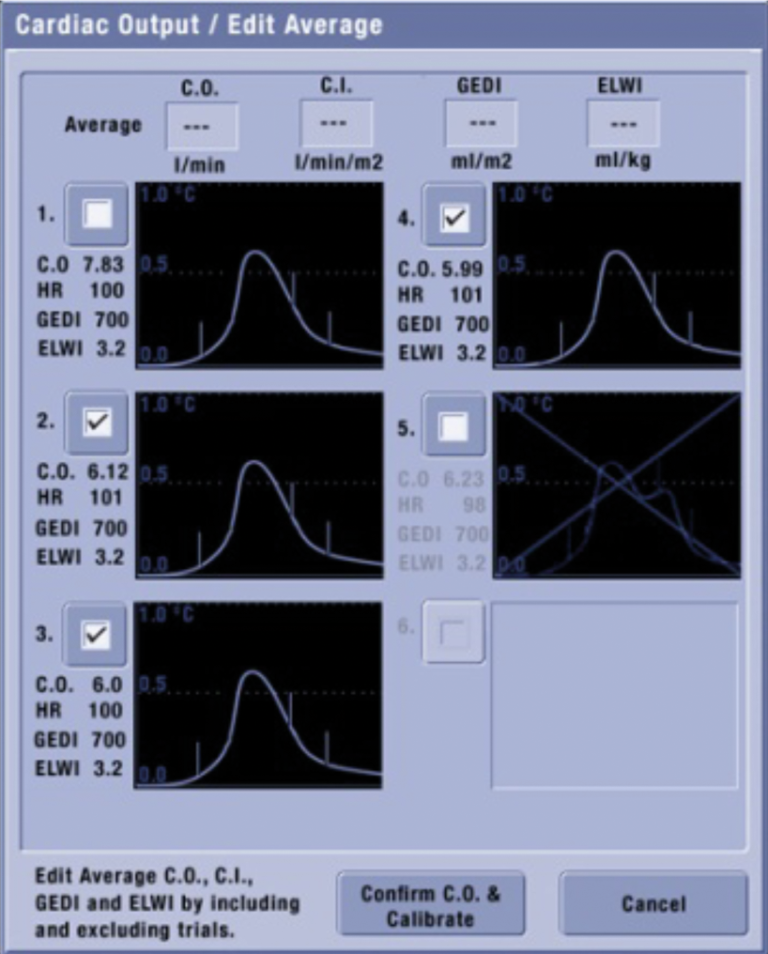
It is important to check ECG, invasive pressures, and temperature while evaluating the C.O. Many factors may influence the C.O. value, for example, injection technique and time between measurements. The injection should be rapid and constant. The curve generated should have a steep rise and gradual return to baseline.
In the PiCCO algorithm, the injection is accepted only if the injection time is short enough. Otherwise the injection is automatically rejected and not considered in C.O. determination.
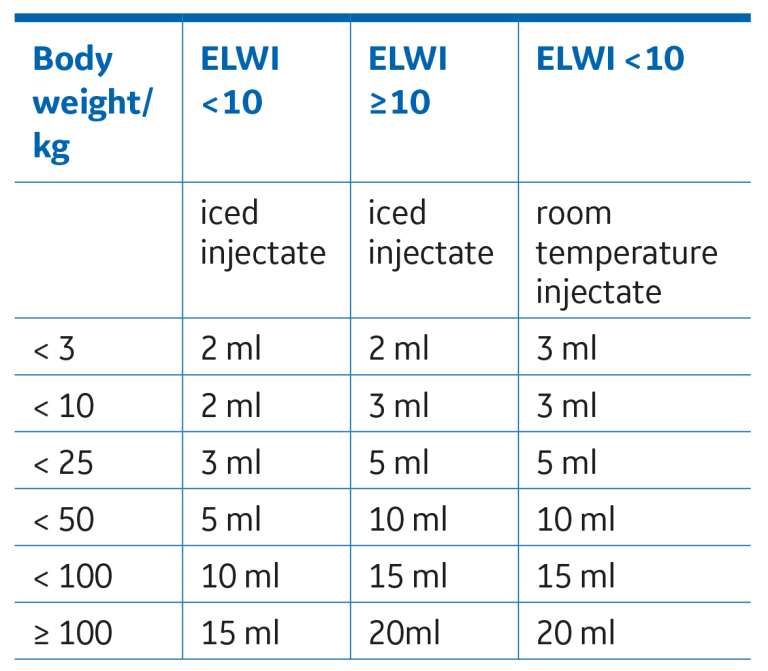
Prolonged injections or excess handling of the syringe can reduce the accuracy of the measurement. An inaccurate injectate volume can cause erroneus calculations. In most cases 10 ml of injectate is enough for a patient weighing 50-99 kg. (110-218lb). The default injectate volume with GE PICCO measurement is 15ml. There are recommended injectate volumes based on patient body weight and injectate temperature, see Table 1.
Rapid changes in heart rate, blood pressure, or pulmonary artery blood temperature may cause irregular curves. Measurements too closely together can also cause errors. Thus, it is recommended to wait five minutes between measurements with iced injectate and one minute between measurements with room temperature injectate.
It is generally recommended to make three to five consecutive determinations with less than 10% variation between the measurements and take the average result. All determinations used for averaging are recommended to be taken within 15 minutes. Irregular curves can be discarded in the Edit Average View of the GE patient monitor before confirming the average result, see Figure 5.
Additional measurements captured
Preload and volume responsiveness
Global end diastolic volume (GEDV) represents the preload volume from all four chambers of the heart, i.e., the volume available to be ejected. GEDV is defined through transpulmonary thermodilution.
Dynamic parameters have been shown to be better tools to assess volume responsiveness than filling pressures.³ Stroke volume variation (SVV) and pulse pressure variation (PPV) are percentage values predicting fluid responsiveness. SVV and PPV are continuously calculated. The higher the value, the higher the probability that fluid loading increases cardiac output. A threshold between 11% to 13% has been reported as predictive of fluid responsiveness.⁴
Global end diastolic volume (GEDV) represents the preload volume, i.e., the volume available to be ejected. In the PiCCO measurement, GEDV actually takes into account the volume of all chambers of the heart. GEDV is defined through transpulmonary thermodilution, whereas stroke volume variation (SVV) and pulse pressure variation (PPV) are continuously calculated.
Afterload
Afterload is assessed with systemic vascular resistance SVR=((MAP-CVP)/CO)*80. It indicates the resistance the heart needs to overcome in order to eject blood to the circulation. Cardiac output is inversely related to systemic vascular resistance (SVR). For instance, vasoconstriction increases resistance, and if there are no changes in other parameters, it leads to decreased cardiac output. It is a continuous measurement with PiCCO technology.
Contractility
Contractility indicates the condition of the cardiac muscle. With PiCCO technology, contractility is defined with cardiac function index (CFI). The formula is C.O. divided by global end diastolic volume.
When preload and afterload have been optimized, the only way to increase
C.O. is to increase contractility by administrating inotropes. CFI is defined by transpulmonary thermodilution.
Extra vascular lung water
When there is an abnormal accumulation of fluid in the extravascular space in the lung, it is called pulmonary oedema. Detection of pulmonary oedema may lead to negative fluid balance. Extra vascular lung water (EVLW) measurement reflects the pulmonary oedema and is an important piece of information when fluid therapy is discussed in hypoxemic patients during mechanical ventilation. EVLW is measured during transpulmonary thermodilution.
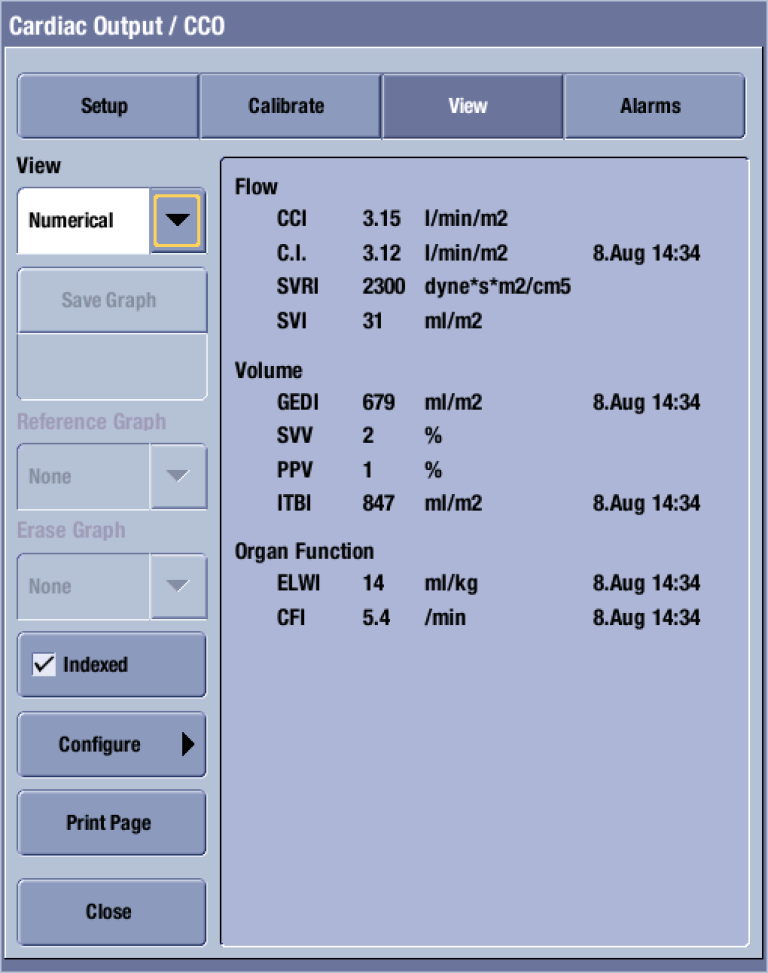
Displaying the information
GE’s CARESCAPE monitors take all of the information the PiCCO technology provides and display it in a graphical view, enabling the clinician to get an overview of the patient's hemodynamic status at one glance†. Parameters shown can be defined by the user, and the coloring of this view is based on the target zone values set by the clinician. see Figure 6.
† Available in CARESCAPE software v2 or later.
Conclusions
Cardiac output is a vital parameter when assessing cardiac function and when making therapy decisions for critically ill patients.⁵ ⁶ C.O. is also routinely measured during and after major surgical procedures.
In addition to continuous cardiac output, PiCCO technology enables other parameters for a comprehensive evaluation of the hemodynamic status of the patient. Using the PiCCO technology is well suited in situations where the hemodynamics are unstable and/or when mechanical ventilation is needed for severe hypoxemia, such as:
- Septic shock
- Cardiogenic shock
- Burns
- Trauma/hypovolemic shock
- ARDS
- Pancreatitis
- Pediatrics
- Perioperative care
References
- Malbrain, M. et al. Cost effectiveness of minimally invasive hemodynamic monitoring, Yearbook of Intensive Care and Emergency Medicine. 603-18,(2005).
- Genahr, A. et al. Transpulmonary thermodilution in the critically ill. British Journal of Intensive Care 6-10 (2004).
- Michard, F. Changes in Arterial Pressuring during Mechanical Ventilation, Anesthesiology, 103, 419-28 (2005).
- Marik, P.E. et al. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: A systematic review of the literature. Critical Care Medicine, 37(9), 2642-7(2009).
- Kirbly & Gravenstein, Clinical Anesthesia Practice, W.B. Saunders Company. St. Louis (1994).
- Sakka, S.G. et al. Measurement of cardiac output: a comparison between transpulmonary thermodilution and uncalibrated pulse contour analysis. British Journal of Anaesthesia, 99 (3), 337–42 (2007).
Additional resources
Arterial Pressure Variation quick guide (DOC0524295) for more information regarding these principles.







