What is gas exchange?
Pulmonary gas exchange measurement, known also as indirect calorimetry, allows continuous and non-invasive measuremen.t of oxygen consumption (V̇O₂), carbon dioxide production (V̇CO₂), and calculation of respiratory quotient (RQ) and energy expenditure (EE).
The gas exchange measurement is used with modular monitors in both anesthesia and critical care areas.
How is gas exchange measured?
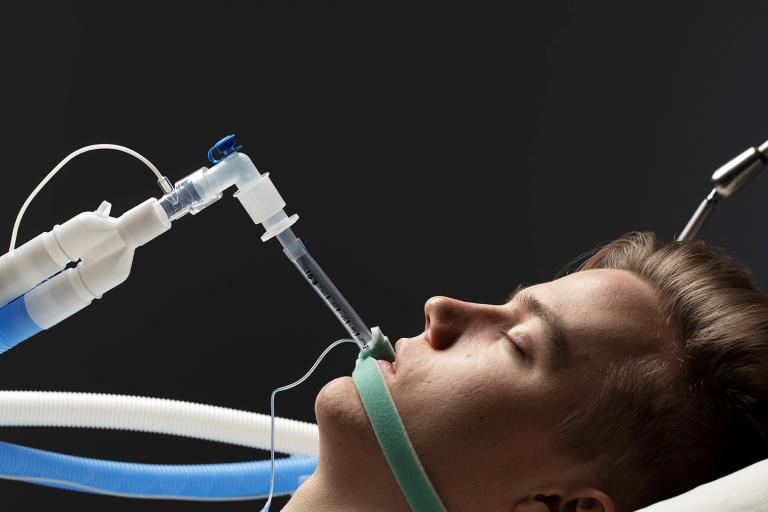
Gas exchange measurement is captured through a gas module and is integrated with both the airway gas and lung mechanic measurements.
Gas exchange information is sampled through a single non-invasive D-lite™ flow sensor and gas sampler at the patient’s airway. Inside the gas module a paramagnetic sensor is used
to measure the O₂ curve and the infrared bench for the CO₂ curve. Both measurements are based on the side-stream principle.
The breath-by-breath measurement of pulmonary gas exchange is technically very demanding and requires sophisticated compensation and data processing algorithms to achieve the accuracy required in the clinical use.
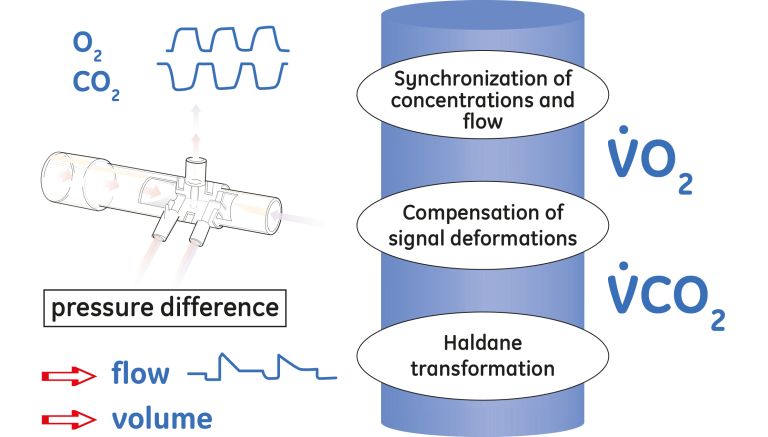
Because of the side-stream principle the measurements of gas concentrations and flow are not simultaneous. When a gas sample passes through the D-lite sensor, the flow signal is recorded with a negligible delay (less than 10 ms) since the pressure difference propagates to the module through the spirometry tubing with the speed of sound. In contrast, it takes on the order of 1.5 s for the gas sample to travel through the sampling line to the module where first its O₂ and then CO₂ concentrations are measured.
The transport time delay is not constant; it must compensate for the fluctuations in the sample flow, variations in the pressure at the D-lite sensor and changes of the gas
concentration. In addition, the finite rise times of the O₂ and the CO₂ sensors need to be compensated utilizing a deconvolution algorithm.
After reconstructing the original waveforms of the gas concentrations and shifting the curves to match the flow signal, the final calculations are based on mathematical integration operation of the product of the flow and each gas signal.¹
The respiratory quotient is calculated from V̇CO₂ and V̇O₂ once every minute and updated to the display also once every minute.
RQ = V̇CO₂/ V̇O₂
The energy expenditure cannot be directly measured, but is calculated from V̇CO₂, V̇O₂ and urinary nitrogen (UN) once perminute.¹
EE = 5.5* V̇O₂+1.7*V̇CO₂ -2*UN
¹ Takala, J. Appliguide, Gas exchange and indirect calorimetry, DOC1305573.
Clinical value
Tool to detect changes in patient’s metabolic status
- Hypermetabolism caused by injuries or septic reactions
Tool for nutritional assesment
- Measurements of energy expenditure and respiratory quotient to avoid under- or over-nutrition
Support in treatment decisions
- Helps to define sufficient oxygen delivery
- Guidance for ventilator settings
- Adequate nutrition
Support in weaning process
- Change in V̇O₂ in weaning trials may indicate work of breathing
- Optimal feeding during weaning
Points to note
- Adequate V̇O₂ / V̇CO₂ values cannot be measured with a leaking airway, with FiO₂ higher than 85%, or when N₂O+O₂ mixtures are used in ventilation or when anesthetic agents are present
- Measurement results are valid only when the respiration rate is below 35/min
- Measurements cannot be taken during the following ventilation modes: high by-pass flow, HFV, BiPAP
- Unstable oxygen delivery may cause erroneous V̇O₂ readings
- Disconnect the D-lite sensor during nebulization of medications to avoid damaging the sensor and contaminating the gas sensors in the module
Simple, easy design
Today’s technology enables an easy, continuous measurement of gas exchange. The bedside module provides for fast set-up without any pre-calibrations, which makes it immediately operational when needed.
The modular design allows for both the hemodynamic and respiratory parameters to be presented on a single screen, which makes the diagnosing of changes fast and easy. Modularity also allows the switching of the module between the patients and brings flexibility and cost efficacy to the treatment.
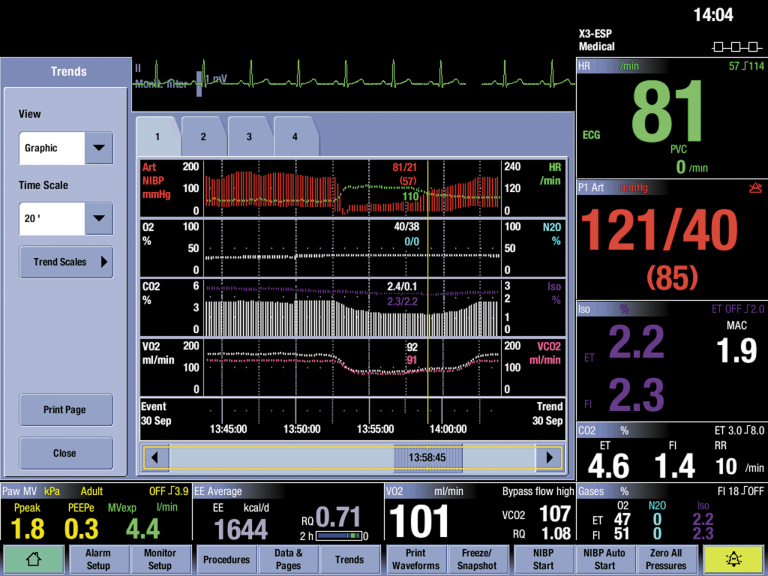
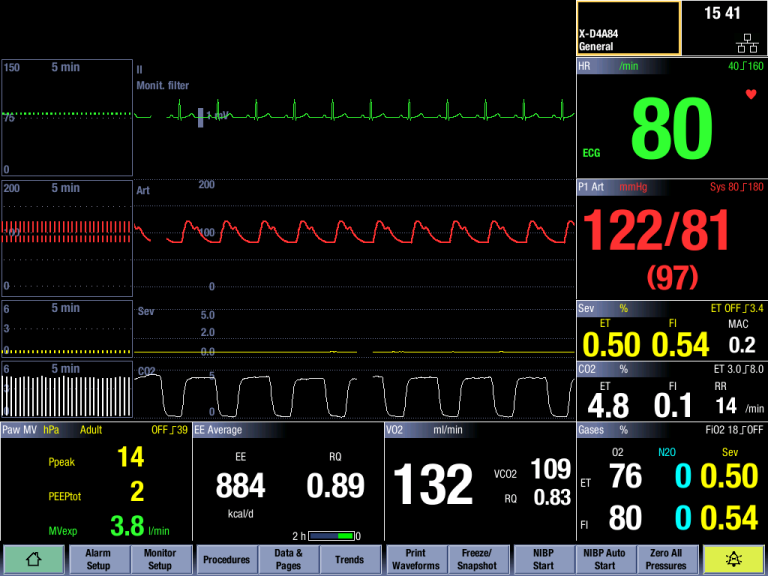
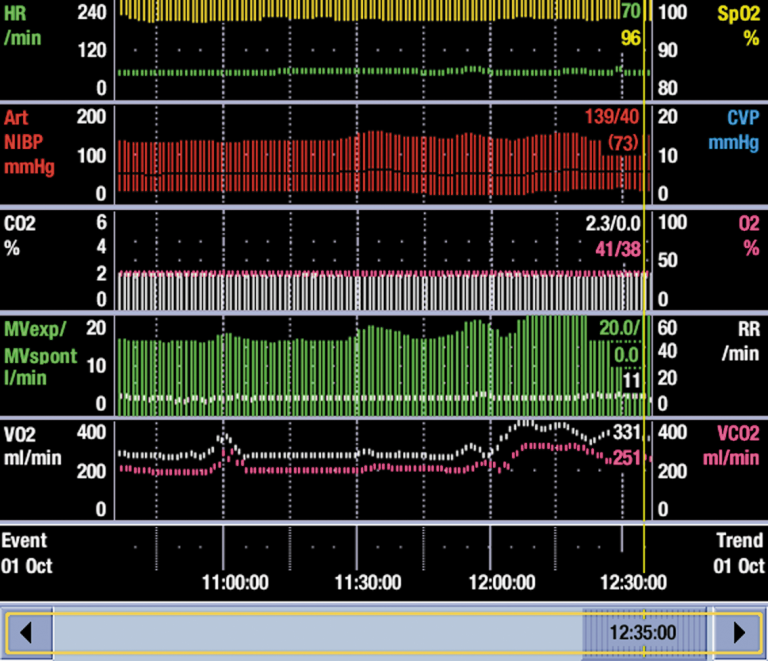
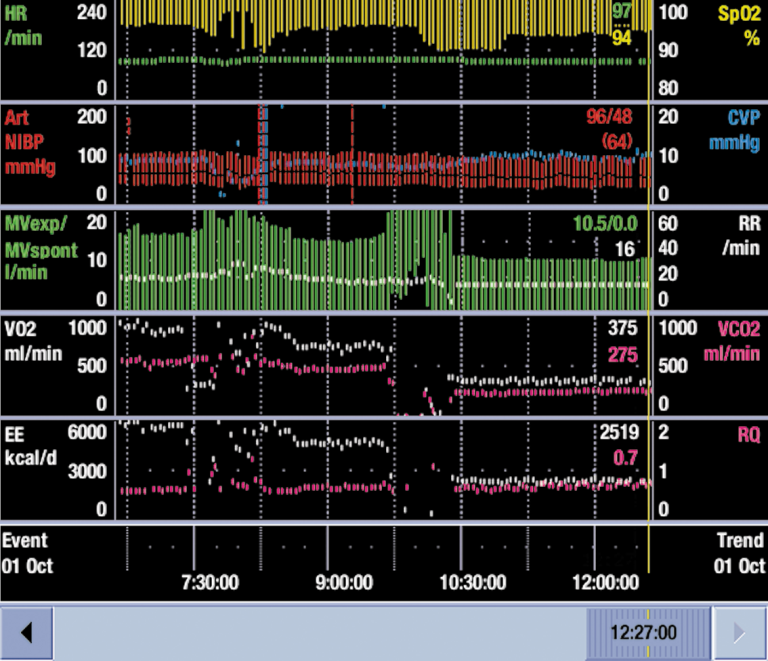
The visible number field continuously shows the actual values, and trend history enables the clinicians to observe and identify changes in patient’s metabolic status.
Clinical examples
In Critical Care
CO₂ production acutely increased from 200 ml/min to more than 300 ml/min. This increase, related to an acute onset of bacteremia, was the sole cause of the increase in ventilatory demand.
Both V̇O₂ and V̇CO₂ increased as an indicator of increased work of breathing when the ventilation mode was changed to pressure support mode (PSV) after controlled ventilation.
In Anesthesia
V̇O₂ decreases rapidly during massive bleeding. V̇O₂ measurement during surgery can be used to estimate the effect of therapeutic interventions.