Background
- Automated gas control is a novel method that alters Fresh Gas Flow (FGF) and controls end tidal agent and oxygen using an End Tidal Control (EtC) device, see Screenshot
- EtC is proprietary software installed on the GE Aisys CS2 anesthesia machine (GE Healthcare, Madison WI).
- The user selects desired end tidal anesthesia agent (EtAA) and end tidal oxygen (EtO2) contentrations. EtAA/EtO2 measured every breath.
- The EtC software algorithm adjusts mixer (FGF) and vaporizer output to achieve and maintain target values, then FGF is automatically reduced to minimal flow when using EtC, to 0.5 L/min
Methods
- A prospective RCT of 220 patients ≥ 18 y, ASA PS 1-3, assigned to Manual Control (MC) or to use EtC to alter FGF and agent/oxygen concentrations automatically. Non-cardiac cases were studied.
- MC arm used standard manual control of FGF or agent/ oxygen, and providers recorded their intended set points.
- EtC arm set the desired EtAA and minimal flow on the Aisys and the EtC software then altered FGF and concentrations.
- Gas data extracted from the Aisys internal log.
- Primary objective; EtC achieves and maintains EtAA and EtO2 in a manner that is non-inferior to MC by a margin of 5%.
- Secondary objectives; safety data for EtC arm, amount of agent used in each arm, number of user interactions.
- Performance of EtC examined percentage of time with agent of oxygen within acceptable concentrations (the greater of ± 5% from steady state mean concentration (SSMC) set), efficacy, response time to reach 90% of the desired SSMC; settling time, time to achieve the desired EtAA and EtO2 SSMC; overshoot, amount the EtAA and EtO2 deviated temporality from final SSMC.
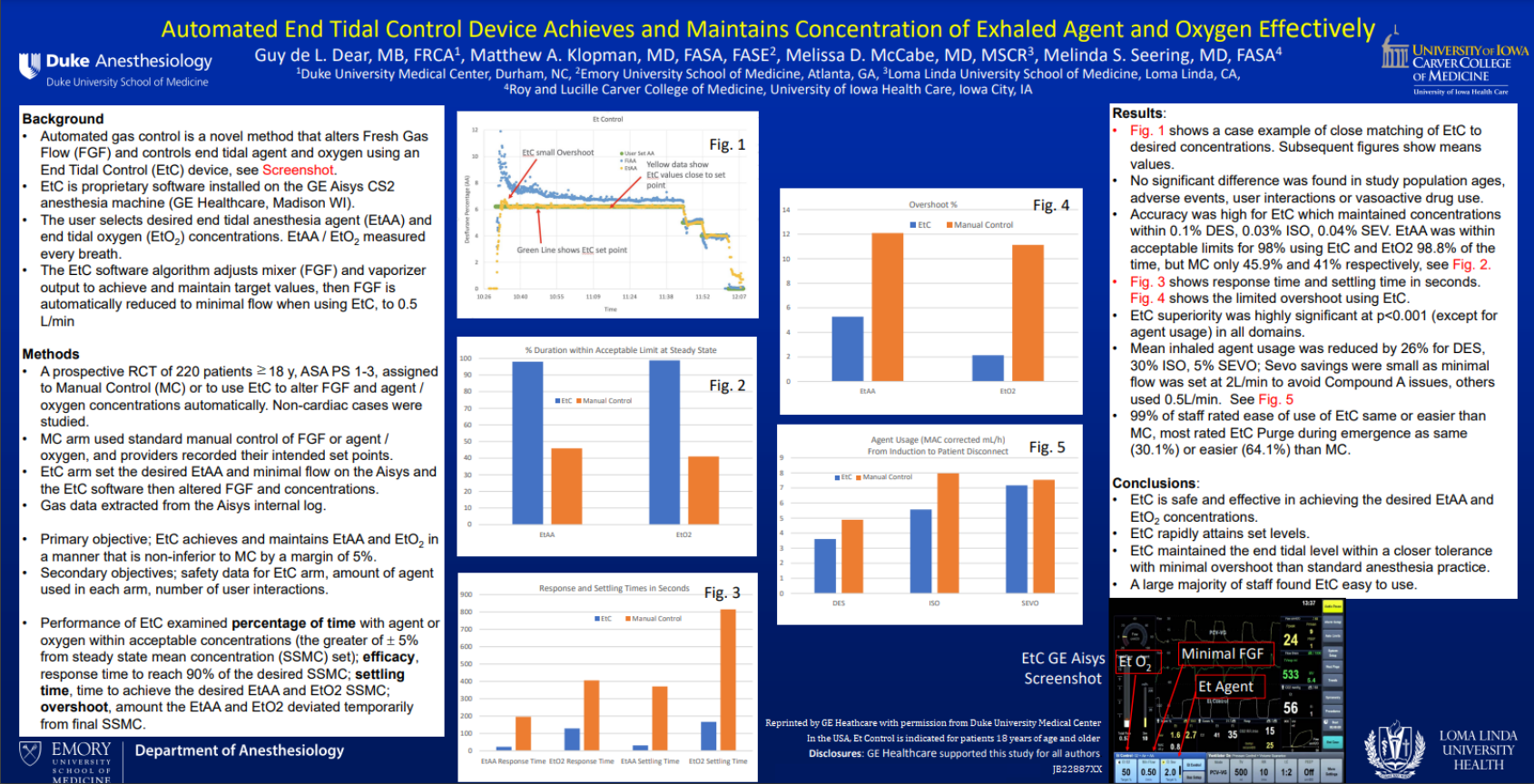
- Fig. 1 : Et Control
- Fig. 2: % Duration within Acceptable Limit at Steady State
- Fig. 3: Response and Settling Time in Seconds
- Fig. 4: Overshoot %
- Fig. 5: Agent Usage (MAC corrected mL/h) from induction to patient disconnect
Results
- Fig. 1 shows a case example of close matching of EtC to desired concentrations. Subsequent figures show means values.
- No significant difference was found in study population ages, adverse events, user interactions or vasoactive drug use.
- Accuracy was high for EtC which maintained concentrations within 0.1% DES, 0.03% ISO, 0.04% SEV. EtAA was within acceptable limits for 98% using EtC and EtO2 98.8% of the time, but MC only 45.9% and 41% respectivesly, see Fig. 2.
- Fig. 3 shows response time and settling time in seconds.
- Fig. 4 shows the limited overshoot using EtC.
- EtC superiority was highly significant at p<0.001 (except for agent usage) in all domains.
- Mean inhaled agent usage was reduced by 26% for DES, 30% ISO, 5% SEVO; Sevo savings were small as minimal flow was set at 2L/min to avoid Compound A issues, others used 0.5L/min. See Fig. 5
- 99% of staff rated ease of use of EtC same or easier than MC, most rated EtC Purge during emergence as same (30.1%) or easier (64.1%) than MC.
Conclusions
- EtC is safe and effective in achieving the desired EtAA and EtO2 concentrations
- EtC rapidly attains set levels.
- EtC maintained the end tidal level within a closer tolerance with minimal overshoot than standard anesthesia practice.
- A large majority of staff found EtC easy to use
In the USA, Et Control is indicated for patients 18 years of age and older
JB22887XX