We all live in a world of data. We have grown accustomed to data access in nearly every aspect of our lives, and it shapes our day-to-day decision-making.
Patient health data is massive but the potential to use it is often locked. If clinicians had access to patient data generated from therapeutic and diagnostic equipment, this could help drive changes in practice and workflow, as well as optimize care.
When hospital systems and administrators attempt to change protocols or practices based on new guidelines – they may struggle because you can’t improve what you can’t (or don’t) measure. Access to data, as well as useful analytics organizing this data, can help improve change management processes.
Studies have found access to real-time feedback from monitoring tools can have a positive impact on change implementation.[1] Productivity increases and costs are reduced when these tools are implemented in the operating room (OR).[2]
As with most things in healthcare, the barriers are multifactorial when it comes to timely and simple access to the right, actionable information. There are gaps when it comes to how data is obtained, retrieved, exchanged, managed, analyzed, and subsequently integrated into clinician workflows.[3] These issues are often related to a lack of functionality despite acknowledgment and investment.3
Consider a seemingly simple improvement initiative that demands a certain behavior change by providers during an anesthesia case to achieve the desired outcome. Accessing the information needed to drive, monitor, and show results of the initiative while also minimizing or eliminating impact on the provider's standard workflow is key to driving adoption and thus success.
However, within existing computer systems it is difficult, sometimes impossible to easily obtain the right, actionable data in an automated fashion. Actionable data can include a variety of data points including measuring the adherence of lung protective ventilation or monitoring the flow of anesthesia gas during surgery. And, of course, without this, displaying the resulting information in a consumable way that can be quickly understood is an impossibility.
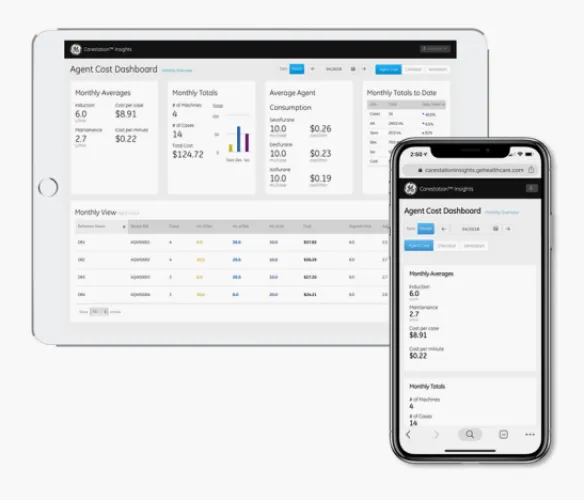
While seemingly daunting issues to tackle, advances in technology and patient data tools, such as digital applications on mobile devices are allowing clinicians and administrators to view and access patient data in ways that are familiar and natural.
Not only do these applications show data in an intuitive way, but they also analyze and organize the high-fidelity data using various analytics and algorithms to provide insights and information, which can eliminate the need for additional manual entries during patient care.
Clinical staff are already overburdened and understaffed – saving time and effort can have a big long-term impact. With these applications, data is now available and compiled in a way that can drive decision-making both in terms of patient care but also workflow optimization.
Today’s article covers some of the benefits of timely high fidelity patient data access and organization and how GE HealthCare’s Carestation Insights applications are supporting clinicians in the OR.
Access to Data Improves Protocol Adherence
Data access and management can help support protocol and best practice adherence. Take, for example, lung-protective ventilation (LPV). LPV strategies are proven to improve clinical outcomes and reduce healthcare resource use in the OR.
But studies have shown implementing these strategies does not always occur, at least not on a consistent basis.[4]
A case study done in France found only 14% of surgical cases used LPV strategies after analyzing more than 2,000 cases over a three-month period. Patient data points were captured and analyzed automatically using the Carestation Insights LPV Application.[5]
After the initial data collection period, an educational campaign was launched focusing on LPV strategies and an LPV implementation protocol was initiated.5
While this campaign was ongoing, LPV strategy implementation improved by 34%.5
Once the behavior and practice were improved, using the Carestation Insights LPV application allowed clinicians and management teams to continue to monitor LPV strategy adherence. This visibility into practice was previously difficult or near impossible to monitor and provides key data points to continue to monitor adherence and identify areas of improvement.5
Data Access Can Help Identify Areas of Improvement
Not only is access to raw data valuable but using intuitive algorithms within the application to help support decision-making is helpful. For example, the Carestation Insights LPV application algorithmically determines patient lung compliance change throughout a case as well as the usage of recruitment maneuvers in order to understand how lung protective ventilation strategies are working in the department.5
While other factors are at play when it comes to change management success – visibility of patient data to drive decision making as well as provide trends in behaviors can play a valuable role.
Identifying areas of clinical practice that could benefit from a change in protocol can be a challenge. Using historical patient data can help management teams find the exact areas in practice that could be improved upon.
One example is monitoring anesthesia agent use. Reducing anesthesia agent use can help reduce cost and reduce the environmental impact of these gases.4 When looking for ways to reduce anesthesia agent use, Dr. Ross Kennedy and his team in New Zealand implemented the Carestation Insights Agent Cost application to discover opportunities for improvement regarding fresh gas flow rates.4
Using the Agent Cost application, data was collected over a three-month period. Researchers were able to identify an area of flow reduction opportunity during the induction phase of anesthesia.4
Data was saved and analyzed, allowing researchers to determine average flow rates during various times.4
Using this data, simple interventions over a two-week period led to behavioral changes in the operating room and subsequent reduction in the duration of high flow gases. There was also significant overall gas usage savings.4
Summary
- Access to live and historical patient data can provide valuable information to both clinicians and management teams
- Access to data as well as analytical tools can improve best practice adherence in the OR
- Identifying areas of improvement is another benefit of effective data collection and management
- GE HealthCare’s Carestation Insights Analytics Applications allow for both live and historical patient data access as well as useful analytics to support clinicians and management teams when it comes to change management and optimizing patient care
References
[1] Hospodkova, P et al. (2021). Change management and digital innovations in hospitals of five European countries. Healthcare (Basel). 9(11): 1508.
[2] Agnoletti, V et al. (2013). Operating room data management: improving efficiency and safety in a surgical block. BMC Surgery. 13: 7.
[3] Islam, M, Poly, T, & Li, Y. (2018). Recent advancement of clinical information systems: opportunities and challenges. Yearbook of Medical Informatics. 27(1): 83-90.
[4] Kennedy, R et al. (2019). The effects of fresh gas flow during induction of anesthesia on sevoflurane usage: a quality improvement study. Anesthesia. 74(7): 875-882.
[5] GE HealthCare (2021). Carestation insights lung protective ventilation (LPV) application case study. https://apps.gehealthcare.com/-/jssmedia/marketplace/products/carestation-insights---lung-protection-ventilation/carestation-insights-lpv-white-paper-us_v3_2021-5_jb03122xx2.pdf?rev=d4495bbde3654d67951c1792ad0fa00b
Data Access Can Help Identify Areas of Improvement
Not only is access to raw data valuable but using intuitive algorithms within the application to help support decision-making is helpful. For example, the Carestation Insights LPV application algorithmically determines patient lung compliance change throughout a case as well as the usage of recruitment maneuvers in order to understand how lung protective ventilation strategies are working in the department.5
While other factors are at play when it comes to change management success – visibility of patient data to drive decision making as well as provide trends in behaviors can play a valuable role.
Identifying areas of clinical practice that could benefit from a change in protocol can be a challenge. Using historical patient data can help management teams find the exact areas in practice that could be improved upon.
One example is monitoring anesthesia agent use. Reducing anesthesia agent use can help reduce cost and reduce the environmental impact of these gases.4 When looking for ways to reduce anesthesia agent use, Dr. Ross Kennedy and his team in New Zealand implemented the Carestation Insights Agent Cost application to discover opportunities for improvement regarding fresh gas flow rates.4
Using the Agent Cost application, data was collected over a three-month period. Researchers were able to identify an area of flow reduction opportunity during the induction phase of anesthesia.4
Data was saved and analyzed, allowing researchers to determine average flow rates during various times.4
Using this data, simple interventions over a two-week period led to behavioral changes in the operating room and subsequent reduction in the duration of high flow gases. There was also significant overall gas usage savings.4
Summary
- Access to live and historical patient data can provide valuable information to both clinicians and management teams
- Access to data as well as analytical tools can improve best practice adherence in the OR
- Identifying areas of improvement is another benefit of effective data collection and management
- GE Healthcare’s Carestation Insights Analytics Applications allow for both live and historical patient data access as well as useful analytics to support clinicians and management teams when it comes to change management and optimizing patient care
References
[1] Hospodkova, P et al. (2021). Change management and digital innovations in hospitals of five European countries. Healthcare (Basel). 9(11): 1508.
[2] Agnoletti, V et al. (2013). Operating room data management: improving efficiency and safety in a surgical block. BMC Surgery. 13: 7.
[3] Islam, M, Poly, T, & Li, Y. (2018). Recent advancement of clinical information systems: opportunities and challenges. Yearbook of Medical Informatics. 27(1): 83-90.
[4] Kennedy, R et al. (2019). The effects of fresh gas flow during induction of anesthesia on sevoflurane usage: a quality improvement study. Anesthesia. 74(7): 875-882.
[5] GE Healthcare (2021). Carestation insights lung protective ventilation (LPV) application case study. https://apps.gehealthcare.com/-/jssmedia/marketplace/products/carestation-insights---lung-protection-ventilation/carestation-insights-lpv-white-paper-us_v3_2021-5_jb03122xx2.pdf?rev=d4495bbde3654d67951c1792ad0fa00b