Clinical value of modular metabolic monitoring early in illness
Case Studies from Edinburgh Royal Infirmary, on an unrestricted research grant.
Dr. Timothy S. Walsh
Consultant in Intensive Care and Anesthesia
Royal Infirmary of Edinburgh
Background
Oxygen consumption and carbon dioxide elimination by the body reflect the metabolic rate of tissues, and the magnitude of aerobic metabolism. Early research in critical illness suggested that oxygen consumption was supply-dependent in the critically ill, but this has now been shown to be unusual in clinically resuscitated patients. Our understanding of oxygen consumption during critical illness has been confused by the problems of accurately measuring this important physiological variable. Historically, the most straightforward and widely used method utilised the pulmonary artery catheter to determine cardiac output, and blood gas data to calculate arterial and mixed venous oxygen content (the inverse/reverse Fick method). This method is time-consuming, intermittent, and subject to considerable measurement error. The Gold Standard for metabolic measurement is gas analysis. Until recently this was only possible with bulky non-integrated systems such as Deltatrac. The COVX module is a new system that is compact, modular, and fully integrated with other ICU monitoring modalities. It measures oxygen consumption and carbon dioxide elimination on a breath-by-breath basis. This new technology offers the opportunity to routinely follow metabolic rate in mechanically ventilated patients.
The critical care oxygen consumption literature is confusing and contradictory, but the following appear to be consistently found:
- Oxygen consumption early in critical illness predicts outcome. Patients with high oxygen consumption are more likely to survive.
- The ability of patients to increase their oxygen consumption in response to a “metabolic challenge”, such as dobutamine, is a strong predictor of outcome. Those that cannot increase oxygen consumption are likely to subsequently die.
- Using oxygen consumption as a target for resuscitation in patients with established critical illness does not appear to improve outcome on an “intention to treat” basis
This information has not been widely used in the clinical management of patients because of the declining use of PA catheters and the inherent errors associated with the oxygen consumption measurements made. The following examples indicate some of the potential of COVX metabolic monitoring early in critical illness.
Case 1
A 72 year-old female patient was admitted to Intensive Care Unit with respiratory failure following abdominal aortic aneurysm repair. Upon admission to the ICU the patient required ventilatory and renal support. The following were observed:
- Sequential Organ Failure Score (SOFA) of 7 (respiratory 3; cardiovascular 1; renal 3)
- High mean oxygen consumption during the first 24 hours (314mLs/min; VO2I 187 mLs/min/m2)
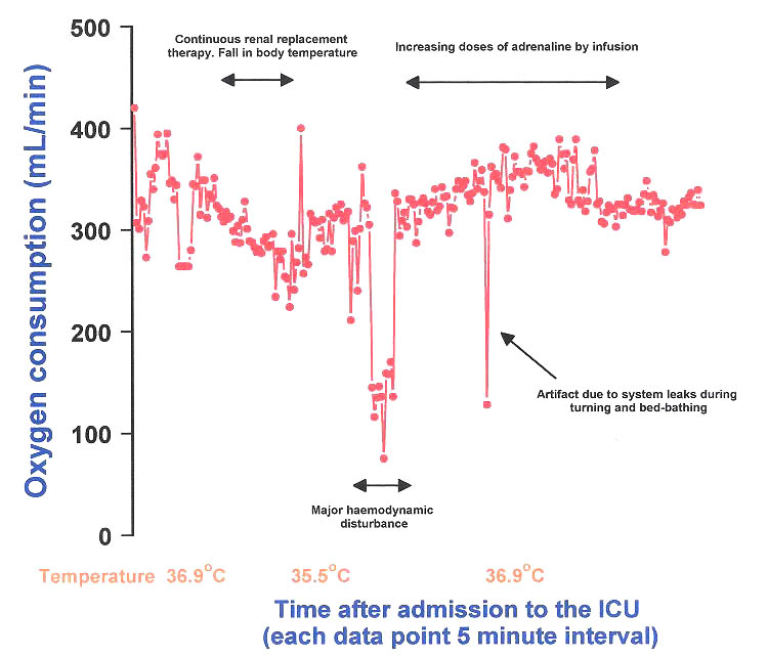
Points of interest from the metabolic data for the first 24 hours:
- Oxygen consumption declined progressively after commencing continuous renal replacement therapy. This occurred in conjunction with a decrease in body temperature from 36.9°C to 35°C, illustrating that metabolic rate in the critically ill changes by about 10% per degree centigrade
- A 30-minute period of cardiovascular instability was associated with profound decreases in oxygen consumption and carbon dioxide elimination. This represented a period of shock and true oxygen supply-dependency
- After commencing adrenaline infusion the patient stabilized and oxygen consumption rose progressively in association with a return of body temperature to normal
By day three the patient had an organ failure score of 13 (resp 3; coagulation 1; liver 1; cardiovascular 4; CNS 0; renal 4). She remained in Intensive Care Unit after 21 days with slowly resolving multiple organ failure.
Case 2
A 74 year-old male admitted post–operatively following laparotomy for faecal peritonitis. On admission the patient required ventilatory and inotropic support. The patient’s past history included ischaemic heart disease, hypertension and longstanding atrial fibrillation. The patient had a SOFA score of 11 in the first 24 hours (resp 3; coag 2; liver 0; cardiovascular 4; CNS 0; renal 2).
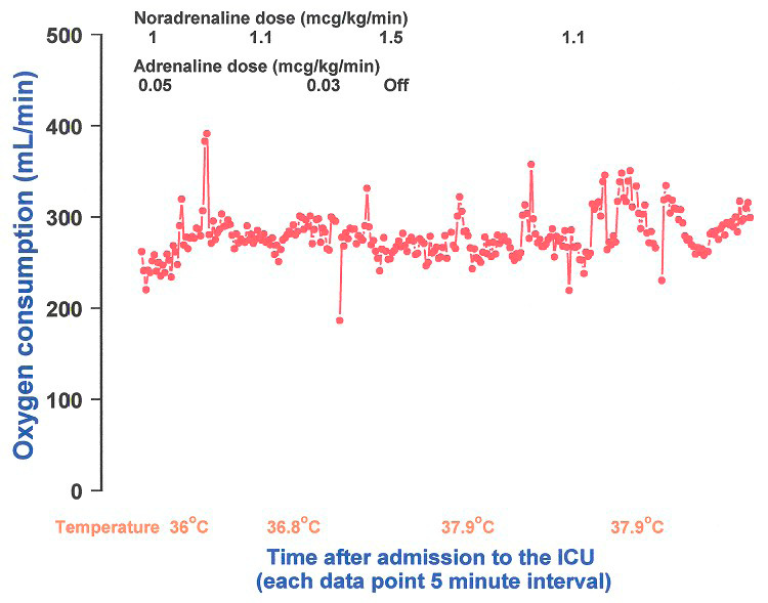
Points of interest from the metabolic data for the first 24 hours:
was the overall very low oxygen consumption during the first 24 hours (mean oxygen consumption 280 mL/min; VO2 index 145 mL/min/m2) and the inability of the patient to increase metabolic rate despite aggressive resuscitation with fluids and inotropes.
The COVX demonstrates these indicators of poor prognosis non-invasively without the requirement of a pulmonary artery catheter. The patient had a prolonged stay in Intensive Care Unit, eventually developed multiple organ failure and subsequently expired after 23 days.
Case 3
A 77 year-old female with a past history of chronic obstructive pulmonary disease was admitted to Intensive Care Unit post-operatively after laparotomy for a perforated diverticulum. The patient was sedated overnight and the following morning sedation was decreased and an attempt to wean from mechanical ventilation was made. The patient’s pre-existing respiratory disease resulted in prolonged weaning, ultimately requiring tracheostomy. The patient required dopamine therapy (2-4μg/kg/min) for cardiovascular support for the first three days in the ICU, but developed no other organ failure. The patient required 11 days of intensive care largely as a result of delayed weaning. Following discharge the patient made a good recovery.
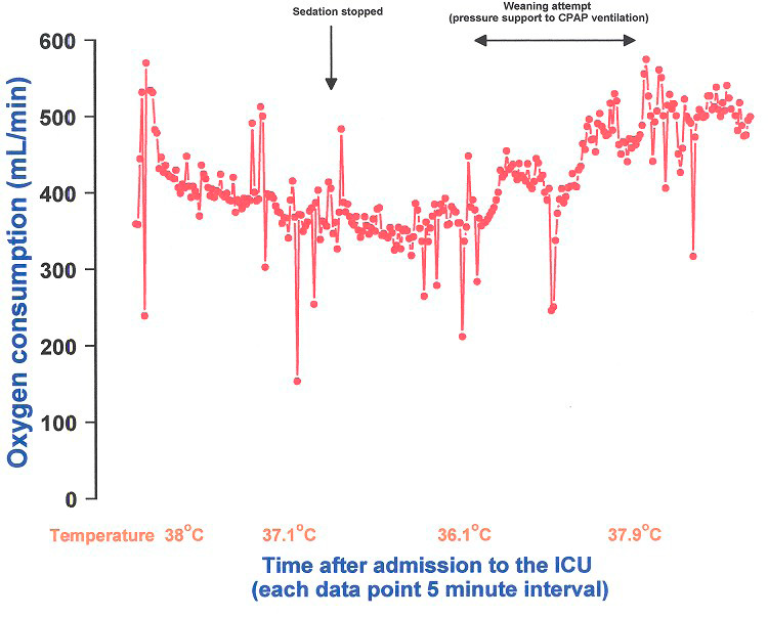
The interesting features of this case were:
- A high oxygen consumption despite sedation during the initial hours in ICU (mean oxygen consumption index 279mL/min/m2)
- An appropriate increase in metabolic rate as consciousness returned after stopping sedation
- The association of these features of good prognosis with absence of other organ failures, and recovery despite significant chronic respiratory disease
The cases illustrate how non-invasive metabolic monitoring provides useful information early in critical illness that relates directly to the response to therapy and chances of subsequent recovery.







