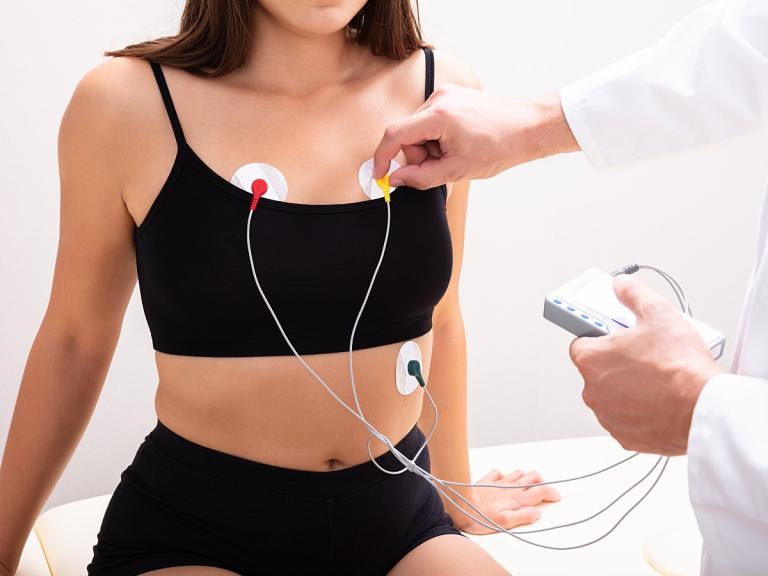
These clinical accessories generate an ECG by connecting adhesive electrodes placed on a patient's chest, arms, and legs to bedside monitors or diagnostic cardiology equipment, allowing for noninvasive monitoring of the heart's electrical impulses.
There are several factors that can impact the accuracy, functionality, and efficiency of an ECG acquisition, including skin preparation and the quality of the ECG leadwires and electrodes. However, the placement of those wires is equally as important. An ECG/EKG machine may come with several leadwires (1, 3, 5, 6, 10). The number of ECG leadwires required depends on the purpose of the ECG recording (monitoring/diagnostic), and the positions will vary based on the purpose.
Misplacing leadwires is common and doing so can have serious implications for a patient's diagnosis.
Achieving Proper ECG Leadwire Placement
Before setting up any electrodes or leadwires, it is critical to properly prepare the skin to assist with signal quality. Skin, specifically the epidermis, is a poor conductor of electricity and can create artifacts that distort the ECG signal. Therefore, electrode sites should be cleaned with either soap and water or an alcohol-free wipe and then completely dried before placement. Electrodes can then be positioned.
Considered the gold standard for monitoring and diagnosing cardiac issues, the 12-lead ECG can also be used outside of the cardiology department—even at a patient's bedside. Six chest or precordial leads allow clinicians to view the heart in the horizontal plane, while four limb leads provide a vertical view. This creates an unparalleled three-dimensional representation of atrial and ventricular depolarization and repolarization that a trained clinician can interpret in just a few minutes.
To best capture this image, the 10 electrodes of a 12-lead ECG should be placed as follows:
Chest Placement
- V1: Fourth intercostal space on the right sternum
- V2: Fourth intercostal space at the left sternum
- V3: Midway between placement of V2 and V4
- V4: Fifth intercostal space at the midclavicular line
- V5: Anterior axillary line on the same horizontal level as V4
- V6: Midaxillary line on the same horizontal level as V4 and V5
Limb Placement
- RA (Right arm): Between the right shoulder and right elbow
- RL (Right leg): Below the right torso and above the right ankle
- LA (Left arm): Between the left shoulder and the left elbow
- LL (Left leg): Below the left torso and above the left ankle
GE HealthCare's high-quality leadwires help set clinicians up for successful placement. Featuring color-coded wires that match up with their corresponding electrode, these innovative clinical accessories ensure accuracy and save time, allowing clinicians to focus on patient care.
These wires also contain shielding that reduces triboelectric noise, which occurs when friction between materials (e.g., a patient gown and a blanket) generates an electrical charge. Triboelectric noise can make it appear as though a patient is experiencing tachycardia when they are not. In turn, clinicians may recommend unnecessary hospitalization or medications, potentially leading to adverse health outcomes as well as avoidable costs for the patient.
Avoiding Improper ECG Leadwire Placement
Imprecise placement can affect the ECG waveform morphology and, in turn, the way a clinician interprets the reading. For example, practitioners commonly place the V1 and V2 electrodes too high, resulting in poor R-wave progression that mimics conditions such as ventricular hypertrophy, notes the Journal of Emergency Medical Services.1 The V1 electrode should be placed to the right of the sternal border, and V2 should be placed at the left of the sternal border in the fourth intercostal space.
V3 is also commonly misplaced, which can affect the shape of the QRS complex, according to a study published in Medical & Biological Engineering & Computing.2 The QRS complex is a combination of the Q, R, and S waves that represents ventricular depolarization. If this complex is interpreted incorrectly, it can lead to misclassifications of arrhythmia or ischemic changes.
Leadwires may also get attached to the wrong electrode, reversed, or placed upside down—all misplacements that can result in poor patient outcomes. Two major factors most commonly lead to incorrect electrode placement:
- Anatomical variation between patients can complicate uniform placement. As an example, there have been conflicting reports about how to place electrodes on patients with large breast tissue; previous guidance recommended placing precordial leads over the breast, but more current research recommends placing them underneath. The latter method reduces the likelihood of altering R-wave voltage.
- Operator error can also play a role in misplacement. Clinicians may assume they know the proper placement—however, they may not have had proper training, or they may multitask while setting up electrodes. Researchers have proposed several methods of controlling variations in electrode and lead placement, including a sliding ruler to facilitate uniformity. However, no solution has been universally employed, so clinicians are still likely to place electrodes and leads subjectively.
The quality of the electrodes in use can also play a role in misplacement. If an electrode has poor adhesive, for example, it may slip out of place or pop off entirely. All placed electrodes should feature low electrode-skin impedance coupled with secure adhesion to ensure good contact and accurate readings. Additionally, ensure that the correct type of electrode is used. A resting ECG and long-term monitoring require different types of electrodes.
Getting an Accurate Diagnosis Every Time
Correct ECG leadwire placement is crucial for making accurate diagnoses and obtaining the best possible patient outcomes. Although ECG usage is common across multiple healthcare settings—so many healthcare personnel understand the practice of placing leadwires and electrodes—frequent training and smart solutions can minimize deviation from proper placement as much as possible.
References
1. Riddle W. Misleading. The clinical implications of misplaced ECG leads. JEMS. 2008;33(9):56-62. doi:10.1016/S0197-2510(08)70320-6
2. Kania M, Rix H, Fereniec M, et al. The effect of precordial lead displacement on ECG morphology. Med Biol Eng Comput. 2014;52(2):109-119. doi:10.1007/s11517-013-1115-9