
In this article, we’ll discuss the benefits of noninvasive respiratory support, as well as the pros and cons of both NIV and HFOT, including the scientific evidence for the use of each therapy. We’ll also take a look at how combining the therapies may benefit patients and whether or not one therapy truly is better than the other when caring for patients with acute respiratory failure.
Reducing complications due to intubation, sedation and infection
Noninvasive respiratory support through NIV or HFOT is considered a first-line treatment for patients with acute respiratory failure and is delivered through nasal cannulas, facemasks or helmets1. Because these devices are external, the pressure and flow they deliver to the upper airways is accomplished without the invasiveness of other options.
The use of these noninvasive therapies offers a number of important advantages over invasive ventilation, including improved safety and outcomes. By avoiding intubation, the support prevents complications due to sedation, eliminates the trauma and discomfort to patient that result from airway insertion and significantly reduces the risk of hospital-acquired infections and healthcare-associated pneumonias1.
Additionally, the improvement in oxygenation that noninvasive respiratory support offers, while protecting the lungs and diaphragm, allows maintenance of cardiac pre-loading and output1. This can lead to fewer patient days in the ICU, and the lower healthcare costs that are linked to a reduced stay1. The use of noninvasive respiratory support also works to preserve patient alertness and interaction, lowering the risk of delirium2. However, which noninvasive option is best for patients suffering from respiratory failure has been a subject of debate, as well as extensive research.
NIV: Improving oxygenation and cardiac function to reduce mortality
NIV is delivered via either biphasic positive airway pressure (pressure support ventilation = pressure support + PEEP on average ranging between 5-8 cmH2O and pressure support of 8-14 cmH2O) or continuous positive airway pressure (CPAP). However, unlike biphasic positive airway pressure, CPAP fails to provide inspiratory support2. Options for NIV delivery include oronasal or full-face facemask (which are considered interchangeable to optimize comfort and tolerance) or helmet interface.
In respiratory failure patients, NIV offers numerous benefits, including increased airway pressure, improved arterial oxygenation, increased end-expiratory lung volume and improved cardiac function due to reduced left ventricular afterload and right ventricular preload2. It also serves to reduce inspiratory effort and the work of breathing for patients2.
A Cochrane Review also combined the results of the largest study to date on NIV along with smaller studies, finding that NIV also significantly reduced hospital mortality3. NIV is widely acknowledged to be a valuable tool for patients with respiratory failure due to1:
- COPD
- Asthma
- Cystic Fibrosis
- Obesity Hypoventilation
The benefits of NIV are also known for patients who present with acute respiratory failure that fall into certain groups including cardiogenic pulmonary edema, postoperative patients and trauma patients3.
HFOT: Increasing patient comfort and guarding the lungs
High Flow Oxygen Therapy is also commonly known as High Flow Nasal Oxygen or HFNO, since it is generally administered via nasal cannula. HFNO delivers heated and humidified high-flow oxygen at a rate of up to 60 L/min, generating a mild PEEP effect2.
Compared with standard oxygen, HFNO offers numerous benefits including reducing inspiratory effort, work of breathing and respiratory rate, and improving comfort and oxygenation2. Studies also show that HFNO may offer more lung protection when compared to standard oxygen by favoring a more homogeneous distribution of tidal volume, in addition to increased alveolar recruitment due to PEEP effect, which may reduce lung strain2.
In patients suffering from hypoxemia, the greatest benefits are generally seen at the highest flow levels2. These benefits make HFNO the optimal strategy for oxygen therapy in patients with acute hypoxemic respiratory failure (AHRF), as well as acute respiratory distress syndrome (ARDS)2.
In a randomized trial with patients that fell into these groups, HFNO reduced intubation rate, while NIV showed no effects on the rate of intubation2. Of additional importance in enumerating the benefits of HFNO is the fact that since HFNO is administered at approximate body temperature and saturated with water vapor, it is generally well-tolerated, and therefore, the negative effects observed with NIV have not been reported with HFNO4.
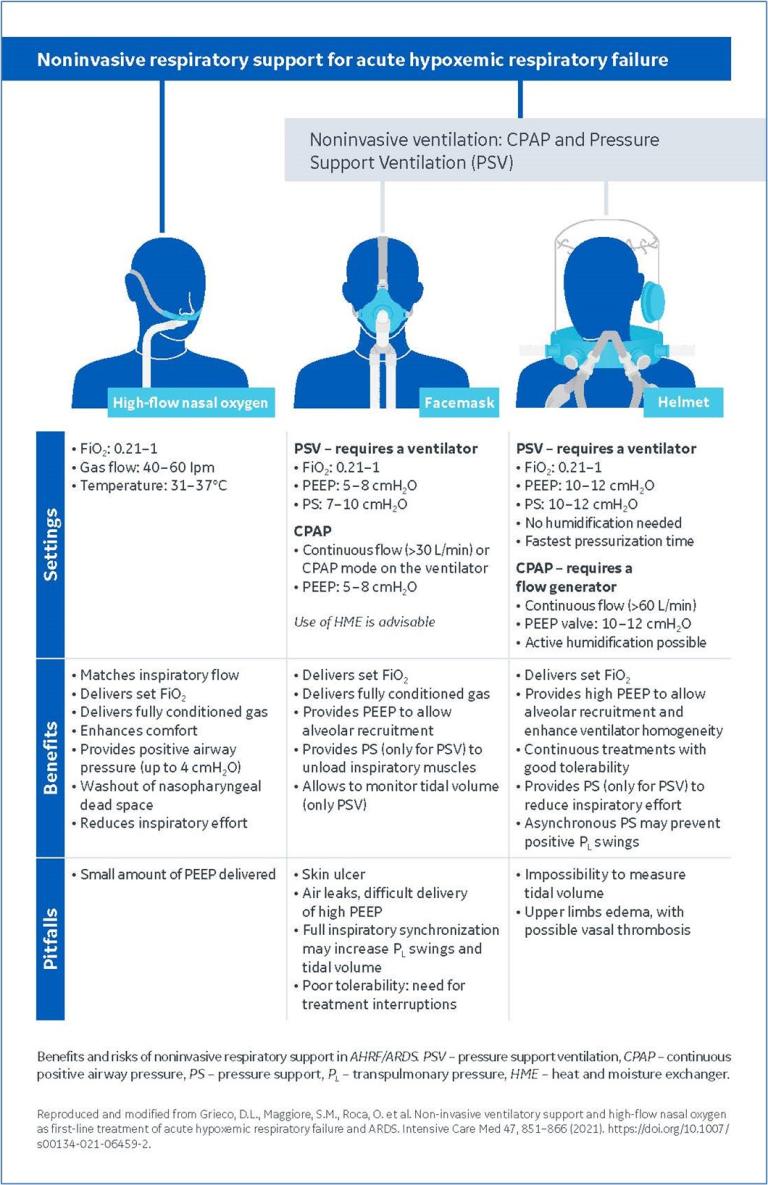
The illustration below illuminates the differences in settings in addition to the benefits and pitfalls of HFNO versus NIV using CPAP or PSV.
Better Together
Clearly, both NIV and HFOT offer significant patient benefits when compared to invasive mechanical ventilation. However, it’s possible that the most extensive benefits of these therapies are better realized when used in conjunction with each other.
In fact, studies are proving that HFNC coupled to NIV could be a way to limit prolonged NIV sessions by maintaining adequate oxygenation between them, while improving patient comfort5.
A study by Frat et al. assessed the comfort, ventilatory parameters and oxygenation levels in patients with AHRF who were treated consecutively with HFNO and NIV showed that5:
- Compared with standard oxygen therapy, PaO2 significantly increased from 83 to 108 mmHg when using HFNO and to 125 mmHg when using NIV, while breathing frequency significantly decreased.
- HFNO was significantly better tolerated than NIV.
The team concluded that HFNO “allowed for significant improvement in oxygenation and tachypnea compared with standard oxygen therapy in subjects with AHRF, a large majority of whom had ARDS. Thus, HFNC may be used between NIV sessions to avoid marked impairment of oxygenation.”
A second study by Spoletini et al. also concluded that HFNO therapy, “had no effect on the duration of NIV sessions or breaks, but it was more comfortable and facilitated eating better than conventional oxygen and prevented the increased tachypnea and dyspnea that occurred with conventional oxygen during breaks1.”
This means that while NIV might be the therapy of choice for certain patient populations, the combination of the two therapies could yield the greatest results.
Summary
- NIV and HFOT serves as first-line treatment of acute hypoxemic respiratory failure and ARDS.
- Compared to invasive mechanical ventilation, these therapies serve to protect the lungs and diaphragm, reduce trauma and discomfort, and prevent hospital-acquired infections.
- NIV offers numerous benefits including reduced inspiratory effort, improved cardiac function and lowered mortality.
- HFOT significantly improves oxygenation and patient comfort, increasing tidal volume and alveolar recruitment.
- Used in conjunction, the therapies may offer even more benefits when HFOT is used as a bridge between NIV sessions to support oxygenation and comfort compared to standard oxygen therapy.
References:
1. Hill, Nicholas, et al. “Noninvasive Ventilatory Support for Acute Hypercapnic Respiratory Failure.” Respiratory Care Volume 64 No 6 (June 2019).
2. Grieco, D.L., Maggiore, S.M., Roca, O. et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensive Care Med 47, 851–866 (2021). https://doi.org/10.1007/s00134-021-06459-2
3. Piraino, Thomas. “Noninvasive Respiratory Support in Acute Hypoxemic Respiratory Failure.” Respiratory Care Volume 64 No 6 (June 2019).
4. Kacmarek, Robert. “Noninvasive Respiratory Support for Postextubation Respiratory Failure.” Respiratory Care Volume 64 No 6 (June 2019).
5. Frat, Jean-Pierre et al. “Sequential Application of Oxygen Therapy Via High-Flow Nasal Cannula and Noninvasive Ventilation in Acute Respiratory Failure: An Observational Pilot Study.” Respiratory Care Volume 60 No 2 (February 2015).
© GE, 2022 – All rights reserved.
GE and the GE Monogram are trademarks of GE. Reproduction in any form is forbidden without prior written permission from GE. Nothing in this material should be used to diagnose or treat any disease or condition. Readers must consult a healthcare professional.
JB18655XX








