
The Enhanced Recovery After Surgery (ERAS) protocol was introduced with the aim of improving perioperative care, minimizing complications and accelerating recovery1. While the ERAS protocol was first introduced in the realm of colorectal surgery, the positive outcomes it generated were soon realized in other specialites2. Today’s ERAS protocols are multimodal-perioperative care pathways designed to achieve early recovery after surgical procedures by maintaining preoperative organ function and reducing the profound stress response following surgery.
In this article, we’ll discuss the multimodal approach to perioperative care ERAS provides, as well as the benefits that can be achieved for both patients and hospitals by embracing the protocol. We’ll also delve into the research that demonstrates the valuable role ERAS plays, regardless of the type of surgery a patient is having.
ERAS then and now
The ERAS protocol is also sometimes referred to as “fast-track surgery” or “fast-track pathway” and was first described in 1997 by Dr. Kehlet4. The main objective of ERAS – to improve patient recovery after surgery – is achieved by putting the patient at the center of their perioperative management and empowering them to accept responsibility in their own recovery plan2.
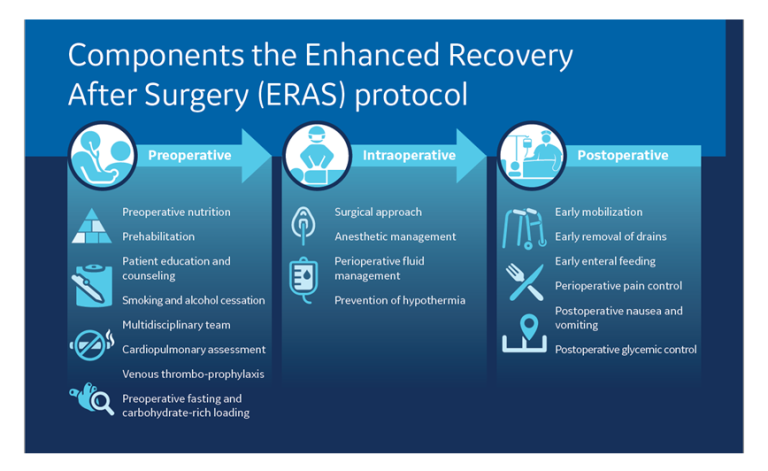
This multidisciplinary management strategy encompasses multiple interventions, while challenging long-held dogmas, like preoperative fasting3. Interventions addressed include preoperative assessment and optimization, patient nutrition, surgical analgesia, the surgery itself and postoperative management2.
The international ERAS® Society has published guidelines for the systematized and validated model, which work to decrease surgical stress, maintain physiological homeostasis and improve postoperative recovery3.
Research now shows that following these guidelines substantially reduces overall costs, length of stay (LOS), postoperative complications, and - according to the article - may be associated with improved long-term survival, while improving the patient experience3. These are benefits which have been achieved not only in the field of colorectal surgery, but also urologic, bariatric, liver, gastric and gynecological surgery and others3.
Let’s take a look at just a few of the studies that back up the benefits of employing ERAS across multiple types of surgery. Please refer to the figure below to see an example ERAS protocol.
Goals of Enhanced Recovery After Surgery Protocols
Lower rate of postoperative complications
One of the most significant benefits of ERAS implementation, no matter the type of surgery, is its ability to reduce postoperative complications.
Joliat et al’s research also included a meta-analysis of 16 randomized trials involving colorectal surgery patients, finding a reduction in postoperative morbidity of 40% with the use of ERAS3. In liver surgery, the authors found that ERAS reduced rates of complications by 30% to 50%3.
In Dai et al’s study involving patients undergoing a Whipple procedure, the ERAS group had4:
- A lower morbidity rate than the conventional group (50% vs. 90.8%; P¼0.00).
- Fewer issues of delayed gastric emptying compared to conventional care patients (0 vs. 11.2%; P¼0.011).
- Reduced incidence of pancreatic fistula – grade B, C – than with conventional care (14.7 vs. 30.6%; P¼0.018)
Research by Kobayashi et al also demonstrated the value of ERAS in reducing complications after surgery, this time in cases of liver resection, with complexity grade as follows: grade I, low; grade II, intermediate; and grade III, high complexity5.
The study included 437 patients where it was found that not using the ERAS protocol was a significant predictor for postoperative complication for every complexity grade.
Shen et al evaluated the impact of the ERAS protocol on patients’ outcomes in benign hysterectomy in 475 women between 2019 and 20206. The researchers classified the women into three groups based on compliance with ERAS:
- Group I: <60%
- Group II: ≥60 and <80%
- Group III: ≥80%
Their results showed that compliance with ERAS resulted in significant reductions in postoperative complications with rates of 20.4% vs. 41.2% vs. 38.1% for groups I, II and III, respectively. Significantly associated with fewer complications were early removal of urinary drainage and early mobilization and oral nutrition.
Finally, Zhou et al’s study aiming to compare the perioperative outcomes of laparoscopic bariatric surgery between patients with ERAS and those with conventional care once again demonstrated the wisdom of ERAS implementation across the surgical spectrum7.
Overall, 435 patients were included with 198 in the conventional group and 237 patients in the ERAS cohort, resulting in a significant reduction of complications in the ERAS group (2.1% vs. 8.6%; P<0.01)7.
Decreased length of stay (LOS)
Research has also shown that implementing ERAS helps to reduce LOS across multiple types of surgery.
Once again, we’ll turn to Dai et al’s work, which looked at the outcomes ERAS offered in Whipple procedure patients. In analyzing LOS, the team found that compared to conventional patients, the ERAS group had a shorter LOS (7.5 vs.12 days; P¼0.00)4.
In a study of 100 patients over the age of 65 who had undergone coronary artery surgery, Çağlı et al found that patients who were under the ERAS protocol benefitted from a significantly shorter intensive care unit stay and decreased time interval discharge8.
Relph et al also found that postoperative hospital stay after vaginal hysterectomy was an average of 42.9 hours in conventional patients versus 23.5 hours in patients who were treated using the ERAS protocol8.
Upon studying the LOS following bariatric surgery in 435 patients, Zhou et al found that the ERAS group had significantly shorter LOS (2.2±0.9 vs. 4.0±2.6days; P<0.01)7. ERAS patients also had a significantly higher day 1 discharge rate (15.2% vs. 1%; P<0.01) compared with the conventional care group7.
Reduced readmissions
The ERAS protocol also shines when it comes to reducing the rate of readmission following surgery.
Zhou et al’s research discussed above found a readmission rate of just 1.3% in ERAS patients after bariatric surgery versus a rate of 4.5% in patients under conventional care7.
Research into ERAS and the likelihood of readmission was also performed by Yilmaz et al in 62 patients undergoing abdominal hysterectomies between December 2016 and February 2017. The authors found that just one (3.3%) patient in the ERAS Group required hospital readmission after discharge compared to 11 (34.4%) patients in the conventional group8.
Reduced costs
Cost reduction is an important advantage of ERAS for both patients and hospital systems.
A review of three studies at a Swiss University Hospital by Joliat et al found that implementation of ERAS accounted for almost $1 million USD in cost savings over just 198 patients3. Additionally, when looking at a provincial healthcare system in Alberta, Canada, the researchers found that utilizing ERAS for colorectal surgery patients netted a cost savings of $2,806 to $5,898 per patient3.
Dai et al also found a net cost savings thanks to ERAS for surgical patients undergoing a pancreatic duodenectomy or a Whipple procedure – one of the most challenging operations in general surgery4. The data on 166 patients in China found that median total hospital cost was significantly reduced in the ERAS compared to conventional patients (¥79,790.40 vs. ¥102,982.81; P¼0.000)4.
Improved patient experience
The final benefit of ERAS implementation we’ll look at is the impact it has on the patient experience.
Following benign hysterectomy, Shen et al found that increased ERAS compliance was associated with higher levels of patient satisfaction and Quality of Recovery Scores (QoR-15)6. In the higher compliance groups, of the five dimensions of the QoR-15, physical comfort, physical independence and pain were improved.
Summary
Although the ERAS protocol was first described for use in colorectal surgery, its value has now been proven across multiple types of surgery, offering important benefits to patients and hospitals. Benefits that can be realized with ERAS include cost reduction, reduced rate of complications and length of stay, lower likelihood of readmission and improved patient experience. This makes it easy to see why the use of ERAS is setting a new standard of care in creating a safe roadmap for the perioperative journey.
References
1: Ashok, Apurva et al. The enhanced recovery after surgery (ERAS) protocol to promote recovery following esophageal cancer resection. Surgery Today (2020) 50:323-334. doi:10.1007/s00595-020-01956-1
2: Jimenez et al. New surgical realities: implementation of an enhanced recovery after surgery protocol for gynecological laparoscopy—a prospective study. Perioper Med (2021) 10: 52. https://doi.org/10.1186/s13741-021-00221-4
3 Joliat et al. Beyond surgery: clinical and economic impact of Enhanced Recovery After Surgery programs. BMC Health Serv Res (2018) 18:1008. https://doi.org/10.1186/s12913-018-3824-0
4: Dai et al. Reducing postoperative complications and improving clinical outcome: Enhanced recovery after surgery in pancreaticoduodenectomy – A retrospective cohort study. International Journal of Surgery (2017) 39:176-181. https://doi.org/10.1016/j.ijsu.2017.01.089
5: Kobayashi et al. Probability of Postoperative Complication after Liver Resection: Stratification of Patient Factors, Operative Complexity, and Use of Enhanced Recovery after Surgery. Journal of the American College of Surgeons (2021) 233 (3):357-368.e2. https://doi.org/10.1016/j.jamcollsurg.2021.05.020
6: Shen, Yiwei et al. Impact of enhanced recovery after surgery protocol compliance on patients' outcome in benign hysterectomy and establishment of a predictive nomogram model. BMC Anesthesiology (2021) 21:289. doi:10.1186/s12871-021-01509-0
7: Zhou, Biao et al. ERAS reduces postoperative hospital stay and complications after bariatric surgery. Medicine (2021) 100 (47): e27831. doi: 10.1097/MD.0000000000027831
8: Yilmaz, Gulseren et al. Enhanced recovery after surgery (ERAS) versus conventional postoperative care in patients undergoing abdominal hysterectomies. Ginekologia Polska (2018) 89 (7): 351-356. doi: 10.5603/GP.a2018.0060
© GE, 2022 – All rights reserved.
GE and the GE Monogram are trademarks of GE. ERAS is a registered trademark of the ERAS Society. Reproduction in any form is forbidden without prior written permission from GE. Nothing in this material should be used to diagnose or treat any disease or condition. Readers must consult a healthcare professional.
JB20450XX














