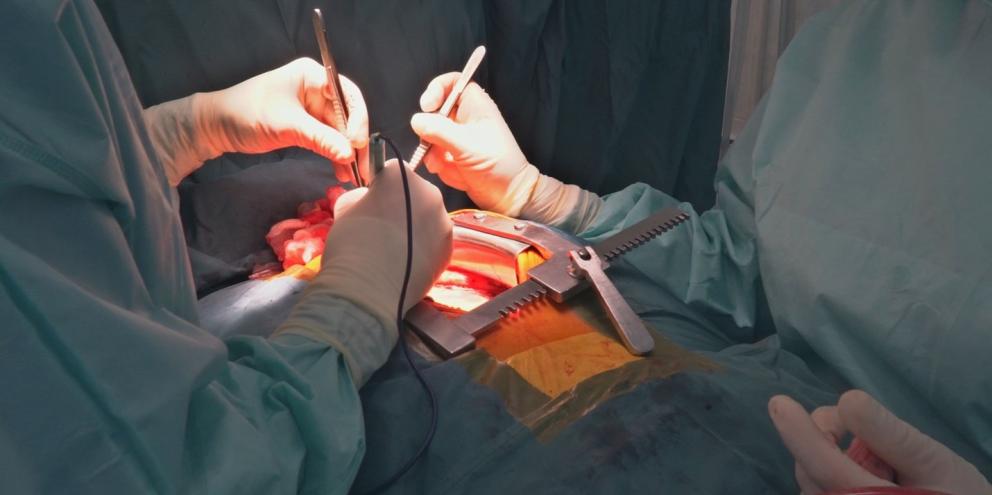
However, the surgery is also burdened by a high rate of postoperative pulmonary complications (PPCs), including pneumonia, pleural effusion and atelectasis, with reported incidence of up to 59.2%1. These are complications that not only prolong the hospital stay for the patient, but also increase in-hospital mortality after surgery and overall mortality1.
Because of these risks, preserving lung function through mechanical ventilation has become a significant field of research, and its use has been long debated. While a number of studies have pointed to the importance of continuing mechanical ventilation, linking the practice to improved oxygenation and postoperative outcomes, other research has found no benefit to the continued use of mechanical ventilation3.
In this article we’ll take a look at the pro/con debate on the use of mechanical ventilation during cardiopulmonary bypass (CPB) surgery. To do this, we’ll break down the state of the current research on whether or not the procedure can improve oxygenation and postoperative outcomes for the 1.25 million patients a year globally who are surgically treated with CPB1.
Looking at the negatives: studies unable to find clear benefits
The majority of the debate around mechanical ventilation during CPB surgery has centered around an inability to conclusively prove its benefits.
For example, in a study of 413 adult patients undergoing elective cardiac surgery with CPB using either no ventilation or low tidal volume (VT) ventilation at 30% or 80% FiO2, Zhang, et al concluded that continuation of low VT ventilation “was not superior to no ventilation during CPB, with respect to incidence of PPCs during hospital stay after surgery”1. However, due to the study design, the authors were unable to draw a strong conclusion for the effects of the application of low VT ventilation at 30% on severity of PPCs.
Another report by Nguyen et al also failed to discover compelling benefits to support the use of mechanical ventilation during CPB2. Their findings, from the MECANO study, a single center randomized clinical trial in patients undergoing cardiac surgery, showed no significant difference in the primary end point, a composite of postoperative mortality and pulmonary complications.
Additionally, a meta-analysis by Shreiber et al, which investigated studies from 1990 to 2010, produced conflicting results. Several trials found that ventilation during CPB using moderate continuous positive airway pressure (CPAP) of 5-10 cmH2O resulted in an improvement in the alveolar-arterial oxygen gradient immediately after weaning the patient from CPB5. In addition, those trials showed that the application of CPAP resulted in an improved oxygenation index and a reduced shunt fraction.
Several of the trials included in the meta-analysis also found that ventilation was more effective than control in narrowing the alveolar-arterial oxygen gradient. Yet, other trials in the analysis found no difference. Only a single trial showed a decreased time to extubation. The balance of the trials discovered no improvements in any index of oxygenation during the immediate postoperative or intensive care period.
Are the positive possibilities enough? Controlling inflammation and improving oxygenation
However, some studies have shown clear clinical evidence that could be achieved through the use of continuous mechanical ventilation for patients undergoing CPB. These studies have pointed to improvements in oxygenation and reduced inflammation that could reduce lung injury.
A recent meta-analysis of 16 clinical trials linked mechanical ventilation (MV) during surgery to a reduced shunt fraction and an increase in oxygenation immediately after weaning from CBP4. Additionally, the determination was made that “maintaining MV during the entire duration of extracorporeal circulation would reduce the CPB-related inflammatory response and resultant tissue damage”.
A second meta-analysis of 17 trials from Chi et al, involving 162 patients found that ventilation during CPB significantly increased post-CPB PaO2/FiO2 ratio and reduced post-CPB alveolar-arterial oxygen gradient (AaDO2)5. The authors concluded that maintaining ventilation during CPB could improve post-CPB oxygenation and gas exchange.
A study by Gaudriot et al, “Immune dysfunction after cardiac surgery with cardiopulmonary bypass: beneficial effects of maintaining mechanical ventilation”, also suggested that maintaining MV during CPB could serve a protective function. The investigators determined that ventilation could help to diminish immune dysfunction and negative immune markers, such as interleukin 10 and tumor necrosis factor-a (TNF-a), after surgery5. This benefit is one that could decrease the occurrence of CPB-related lung injury.
Finally, Loeckinger et al presented compelling results supporting the use of mechanical ventilation. After comparing CPAP at 10 cmH2O during CPB with deflated lungs6. Their findings showed that “higher CPAP improved ventilation-to-perfusion ratios for all lung areas observed” and that PaO2 levels remained significantly higher in the CPAP group compared with the non-ventilated group four hours post-CPB. Of significance, the researchers also noted a trend toward earlier extubation in the CPAP group. The authors postulated that the atelectasis and shunting that occur with ventilation cessation was prevented by the higher airway pressures.
Getting to the core of patient safety
While the debate over the use of mechanical ventilation during CPB is ongoing, there is clear evidence that cessation of ventilation can lead to atelectasis and decreased surfactant production and is associated with both systemic and pulmonary inflammation4. Considering that numerous studies have linked ongoing mechanical ventilation to improved oxygenation and reduced inflammatory markers, future studies could demonstrate that continuing ventilation could serve to improve patient safety, reducing PPCs, length of hospital or intensive care unit (ICU) stay and mortality.
References:
1. Zhang, Meng-Qui, et al. “Effect of ventilation strategy during cardiopulmonary bypass on postoperative pulmonary complications after cardiac surgery: a randomized clinical trial.” Journal of Cardiothoracic Surgery Vol. 16:319 (2021). https://doi.org/10.1186/s13019-021-01699-1.
2: Schultz, Marcus, et al. “Ventilation During Cardiopulmonary Bypass: Can We, Must We, Should We Individualize It?.” Chest Vol. 159, Issue 5 (2021).
3. Dryer, Chinwe, et al. “Con: Mechanical Ventilation During Cardiopulmonary Bypass Does Not Improve Outcomes After Cardiac Surgery.” Journal of Cardiothoracic and Vascular Anesthesia Vol. 32 (2018).
4. Bignami, Elena, et al. “Different strategies for mechanical VENTilation during CardioPulmonary Bypass(CPBVENT 2014): study protocol for a randomized controlled trial.” Trials Vol. 18:264 (2017).
5. Chi, Dongmei, et al. “Ventilation during cardiopulmonary bypass for prevention of respiratory insufficiency: A meta-analysis of randomized controlled trials.” Medicine Vol. 96:12 (2017).
6. Bhatia, Meena, et al. “Pro: Mechanical Ventilation Should Be Continued During Cardiopulmonary Bypass.” Journal of Cardiothoracic and Vascular Anesthesia Vol. 32 (2018).
© GE, 2022 – All rights reserved.
GE and the GE Monogram are trademarks of GE. Reproduction in any form is forbidden without prior written permission from GE. Nothing in this material should be used to diagnose or treat any disease or condition. Readers must consult a healthcare professional. JB18654XX