The operating room (OR) is an area constantly being pushed to the limits of efficiency, productivity, and clinical excellence. This can lead to continuous cycles of change in both clinical guidance and standards as well as operational workflows.
Research has shown how small interventions, even those that don’t require additional resources, can drive continuous improvement in the OR. Improvements in both the use of the OR and staff satisfaction can be achieved with well-placed interventions.[1]
However, in reality, staff shortages, budget constraints, limitations to accessible data, and time to analyze are all barriers that can make lasting change and adherence difficult to achieve even when there is strong evidence.
Access to Data
Data collection is an important part of the patient picture when it comes to decision making and delivering high quality care. Data includes vital signs and imaging as well as historical information (OR and ICU visits, etc.).
Not only is data collection itself a challenge, access to the right data to drive decision making is difficult. Data analysis and retrieval requires many resources that are costly and time consuming – and even if it is completed – providing this detailed data to clinicians in a timely and sustainable manner has proven to be difficult.
Additionally, many data analysis and retrieval programs and systems tend to provide very complicated patient data reports with a lot of extraneous information, leading to confusion that ultimately impacts any chance of driving change quickly.
Providing clinicians simple access to the relevant data has proven to be a barrier to care in the hospital setting highlighting the need for improvements in data collection and sharing.
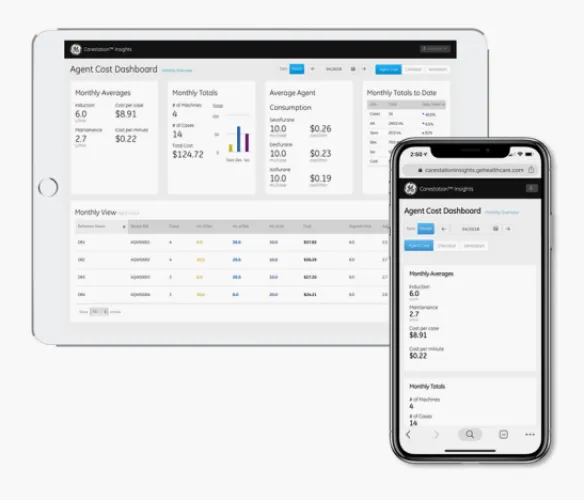
It’s been shown that when hospital operational level administrators anesthesiologist administrators can visualize patient and operational information, operating room efficiency and patient safety can improve.[2]
Specific OR Scenarios and Challenges
Lung protective ventilation, low flow anesthesia, and the use of quantitative monitoring when using neuromuscular blocking agents are a few areas that even with strong evidence backing their use in the OR, have been shown to have low adherence as well as slow adoption.
The use of standardization through implementing protocols and ensuring that there are measurements to track protocol adoption and success, are ways to expedite adoption and support clinicians in using best practice.
Lung Protective Ventilation
Lung protective ventilation (LPV) has been shown to help reduce pulmonary complications in the OR3. As a rapidly developing technology, there have been barriers to adherence regarding LPV and PEEP strategies.
Researchers have found when protocols as well as clinical decision support (CDS) tools were used, adherence of LPV is increased. CDS tools were felt to be easy to use and respiratory therapists (RTs) at high-adherence facilities said the tools increased their self-efficacy when applying LPV strategies.[3]
Standardized LPV tools and protocols were also reported to increase responsiveness to patient needs in facilities with high-adherence to LPV practices. It’s important to note the same study reported RTs saying the CDS tool limited their autonomy in low-adhering sites.3
Knowing that a protocol and CDS tool can be perceived as both helpful as well as less than helpful is important to recognize when developing and implementing new protocols. It’s finding the delicate balance in supporting clinicians in their OR tasks versus hindering their progress that is the challenge.
Low Flow Anesthesia
Healthcare services account for 5% of all greenhouse gas emissions with a large portion of them coming from the operating room and anesthesia services.[4]
Utilizing low flow anesthesia practices can help reduce overall greenhouse emissions. Thanks to advances in anesthesia device technology, utilizing low flow is easier to accomplish, but research has shown there is room for improvement when it comes to standard implementation.[5] [6]
Lack of awareness of the environmental issues surrounding inhaled gases has been cited as a barrier to implementation as well as lack of ideal monitoring technology.6 In order to safely use low flow anesthesia, strict monitoring of oxygen use, agent analyzers, monitoring inspired and expired CO2 as well as other parameters are needed – all of which were reported to be minimally monitored currently.
As with other initiatives to improve adherence surround change management practices, more access to information is key to increase implementation. A 2019 study found that when clinicians have access to monthly measures of gas flow, volatile agent use, and even how many bottles of volatile agent were purchased, low flow use was increased and department costs were reduced.[7]
Clinicians had access to pictorial and graphical representations on a ‘low-flow board’ and this resulted in 18% fewer bottles of volatile agents being ordered despite an increase in patient load.7
Two ways that may improve low flow anesthesia use are better monitoring technology as well as increasing data collection and sharing among clinicians.
NMBA Monitoring
Neuromuscular blocking agents (NMBAs) are used both in the OR and in the ICU and require vigilant monitoring to reduce adverse events. Historically, monitoring consists of subjective measuring which has proven to not always be reliable.
Quantitative monitoring devices including acceleromyography and electromyography can help reduce morbidity while using NMBAs intraoperatively. Monitoring is crucial intraoperatively as well as during the awakening period to ensure proper resolution of the effects of NMBAs.[8]
NMBA monitoring application is another area that has proven to be challenging when it comes to consistent adherence regarding change management and use in the OR.8
When surveyed, anesthesiologists felt the lack of training, unreliable equipment, and a lack of standards or guidelines contribute to barriers when it comes to consistent use of neuromuscular monitoring. Clinicians reported difficulty calibrating monitors and interpreting measurements at times.8
Logistical barriers including cable storage for monitors and faulty barriers contributed to a decrease in monitoring use.8
Clinicians reported increased adherence when NMBA monitoring devices were integrated into other anesthesia machines and equipment highlighting the benefits of using a device that can complete multiple functions beyond NMBA monitoring.8
These challenges further highlight the benefit of using protocols and guidelines that can be incorporated within monitoring devices as well as the need for user-friendly devices to increase adherence.
Summary
- The OR is a place constantly evolving and changing due to an ever-present drive to increase efficiency and patient safety while utilizing as few resources as possible
- Improving clinician and administrative access to high fidelity patient data can facilitate change management and improve efficiency
- Standardization via protocols integrated into device along with measurable and trackable guidelines can help facilitate change management
- LPV, low flow anesthesia, and NMBA monitoring are areas that could benefit from improvements in both communication and standardization to improve adherence
References
[1] Sandbaek, B, et al. (2014). Impact of changed management policies on operating room efficiency. BMC Health Services Research. 14. 224
[2] Agnoletti, V. (2013). Operating room data management: improving efficiency and safety in a surgical block. BMC Surgery. 13(7).
[3] Knighton, A et al. (2020). Multi-factorial barriers and facilitators to high adherence to lung-protective ventilation using a computerized protocol: a mixed methods study. Implementation Science Communications. 67.
[4] Drew, J et al. (2021). Operating in a Climate Crisis: A State-of-the-Science Review of Life Cycle Assessment within Surgical and Anesthetic Care. Environmental Health Perspectives. 129(7). 076001-1–076001-18.
[5] Ryan. S. (2012). Sustainable Anesthesia. International Anesthesia Research Society.114(5). 921-923.
[6] Amma, R et al. (2016). A survey on the use of low flow anesthesia and the choice of inhalational anesthetic agents among anesthesiologists in India. Indian Journal of Anesthesiology. 60(10): 751-756.
[7] Carter, L et al. (2019). Promoting low-flow anesthesia and volatile anesthetic agent choice. BMJ Open Qual. 8(3): e000479.
[8] Thomsen, J, et al. (2020). Barriers and aids to routine neuromuscular monitoring and consistent reversal practice- a qualitative study. Acta Anaesthesiologica Scandinavica. 64(8):1089-1099.