
Fetal lung development is a process that continues right up until full gestation.1 Because of underdeveloped lungs, the premature infant often requires respiratory support to ensure oxygenation of the tissues and organs as the baby grows.
Underdeveloped lungs require oxygen, making supplemental oxygen being the most common ‘drug’ used in the Neonatal Intensive Care Unit (NICU).2
While vital in many cases, over-oxygenation (hyperoxemia) contributes to a handful of problems in neonates. Over oxygenation leads to Retinopathy of Prematurity (ROP), bronchopulmonary dysplasia, and neurodevelopmental impairments in premature infants.3
Monitoring oxygen saturation (SpO2) in premature infants is a standard clinical practice and this includes achieving targeted oxygen saturation after delivery and clinically set ranges for infants in the NICU.3
Histogram data helps provide a bigger picture of oxygen saturation and the respiratory support needed by the infant over an extended time period. Histograms include analyzing the range of oxygen and fluctuation outside of the desired ranges.
The histogram creates a pictorial of the analysis over time, showing the percentage of time the patient was within a defined range of oxygen limits. This data may be used when assessing infant responses to oxygen therapy and respiratory support in real time or trended over a period of time.3
Today’s article reviews what histogram data provides and how these graphs can support clinicians when it comes to supplemental oxygen and respiratory support management in the newborn patient.
What is a Histogram?
Histogram data is made up of ECG (heart rate), SpO2 (pulse oximetry) and from impedance respiration or end tidal CO2 (respiration rate) measurements.3
From this trended data, percentages are made reflecting the time an infant spent in a certain oxygen saturation or heart rate ranges.3
Oxygen saturation range readings are represented as a graph, typically a bar graph, to illustrate the time spent in or out of a set range, for example how often and long were they in the 94-95% oxygenation range.[4]
The benefit of using a graph rather than a listing of percentages means histograms are easier to evaluate for trends as well as real-time assessments.4
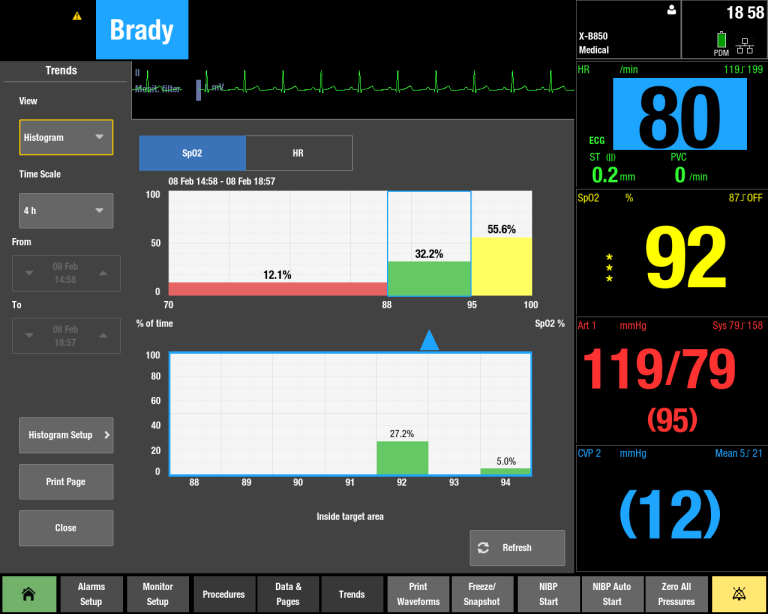
Another benefit of histograms is parameters can be customized based on patient status or clinician preference. Clinicians can evaluate trends over minutes or hours, as well as create range sets for oxygen saturation.4
Histograms as a Tool of Prediction
There are no concrete instructions when it comes to weaning infants off continuous positive airway pressure (CPAP) or ventilator support and supplemental oxygen. Typically, the clinician’s experience and assessment of the overall clinical picture including gestational age, respiratory effort, and FIO2 requirements are used to provide a general guidance when it comes to altering oxygen or respiratory support.3
Histograms provide a more complete picture of respiratory support in the neonatal population. Not only is there more information about current oxygenation status, but histograms bring predictive value to clinicians in the NICU.3
Histograms can also be used to help determine if an infant is ready to be weaned off CPAP or other respiratory support.3
Several studies have monitored histogram data and trends and the subsequent neonatal outcomes:
- One such study evaluated histogram data in the 24 hours prior to transitioning from invasive oxygen delivery modes to less invasive ventilation and less oxygen. Researchers found if an infant (24-32 weeks gestational age) spent 15% (or more) time with pulse oximetry readings <86% during the 24-hour period, they were more likely to fail the transition to low-flow nasal canula, oxyhood, or room air.3
- A 2021 study looked at SpO2 histogram data in 60 preterm infants (ranging from 23 weeks and 33+6 weeks gestation) that required respiratory support. When exploring correlations between histogram profiles, researchers found a strong correlation between 4- and 24-hour histogram readings. By determining this correlation, clinicians were better able to predict an infant’s response to any changes made regarding respiratory management.2
- A 2020 study explored the accuracy of this prediction in infants born at or before 30 weeks’ gestation or weight less than 1250 grams at birth.[1] The study found if an infant achieved target oxygen saturations for a set period of time prior to CPAP being discontinued, this data point was an accurate predictor of CPAP weaning success.5
Each of these studies show promise for the development of objective data points to guide oxygenation support in this patient population. While the whole patient picture should always be considered, having meaningful data and trends like histograms can lead to better patient outcomes.
There is clear evidence that demonstrates and supports the benefits of incorporating histograms in clinical practice. Two such benefits cited by the Sur and Paria (2020) study include using histograms to predict the readiness for respiratory support transition and predicting escalation needs of the infant.4
Histogram Impact on Clinical Outcomes
A study of over 500 neonates concluded when clinicians implemented histogram training and monitoring, the rates of severe ROP or death decreased from 32.1% to 18%. This study also found infants spent more time within their goal saturation with histogram monitoring (48.7 – 57.6%).4
In addition, the use of histogram data helped show these same infants spent more time within their set saturation goals (48.7-57.6%).4
Another study focused on retinopathy of prematurity found that histogram analysis implementation decreased the odds of severe ROP and decreased the rates of retinopathy that required surgery.4
Finally, a 2019 review of 75 neonates found that when histogram analysis was documented, infants at risk for prolonged respiratory support were identified earlier.4 Histogram graphs were also found to be more accurate when compared to manual documentation of data points.4
Using automated tools like histogram have been shown to be more accurate than manual documentation of data points when it comes to respiratory events and also leads to fewer instances of needing to manually document. Researchers concluded this could help save clinicians time and increase precision care in a busy acute care setting.4
While more research is needed around the utility and role histogram graphs and analysis ultimately play in the NICU, it is clear this data provides valuable information about respiratory status in the premature population. Using histogram data, heart rate, and SpO2 can identify optimal ranges that allow clinicians to promptly identify treatment plans which can positively impact the infant’s outcome.
Summary
- Supplemental oxygen is vital yet complex in the neonatal setting
- Histogram readings provide objectivity of infant reactions to respiratory support, including supplemental oxygen
- Histogram analysis has shown to improve patient outcomes including weaning success as well as reducing adverse events in neonates
References
[1] Rehman, S & Bacha, D. (2021). Embryology, pulmonary. NCBI StatPearls.
[2] Pringleton, H. & Loganathan, P. (2021). Role of oxygen saturation histogram profiles in predicting hypoxemia and hyperoxemia in premature infants. Archives of Disease in Childhood. 106. A20-A21.
[3] Mense, L & Waitz, M. (2016). Spo2 histograms in preterm infants: a helpful tool for neonatologists? Respiratory Care, 61(4). 569-570.
[4] Sur, A & Paria, A. (2020). Histogram analysis for bedside respiratory monitoring in not critically ill preterm neonates: a proposal for a new way to look at the monitoring data. Eur J Pediatr. July 8. 1-7.
[5] Gentle, S, Ambalavana, N, & Carlo, W. (2020). Oxygen saturation histograms predict nasal continuous positive airway pressure-weaning success in preterm infants. Pediatric Research. 88. 637-641.








