Unfortunately, this experience actually happens to patients, and it's one anesthesiologist always hope to avoid. Patient safety is always the primary concern for any anesthesiologist, but the patient experience isn't far behind. Awareness and recall can be traumatic for patients and lead to a suboptimal experience. Conventional cardiac and pulmonary measures are not completely reliable for ascertaining the level of hypnosis in patients undergoing general anesthesia, and the effects of general anesthesia on the brain are not yet fully understood.
However, advances in monitoring have been gamechangers for assessing patient depth of anesthesia.
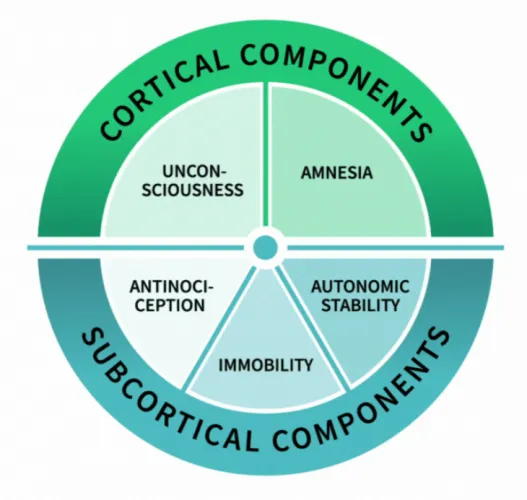
Advanced depth of anesthesia monitoring assesses the effects of anesthetic drugs on the brain using electrode sensors applied to the patient’s forehead. This noninvasive system measures the degree of irregularity (depth of anesthesia) in electroencephalograph (EEG) signals, based on the general association between changes in EEG entropy and changes in the cerebral cortex. In adult patients, high entropy values (high irregularity in the signal) indicate that the patient is awake. Low entropy values (low irregularity in the signal) are associated with a likely lack of consciousness.1
Compared with standard clinical monitoring during general anesthesia, depth of anesthesia monitoring is associated with additional costs. Depth of anesthesia monitoring requires purchasing specialized equipment, including electrode-bearing sensors. Costs also include training for the relevant clinical staff in the use of depth of anesthesia-monitoring technology, as well as facility-related operational costs, such as updating protocols.
Depth of anesthesia monitoring can be helpful in guiding the clinician in administration and titration of anesthetic drugs, which may lead to an improvement in the quality of care and reduction in anesthesia costs and overall healthcare costs. In particular, EEG-based monitoring may be able to mitigate the occurrences of overdosing and underdosing.
Overdosing can result in high medical costs for various reasons. These include greater/unnecessary use of anesthetic drugs; slower patient emergence, awakening, or extubation in the operating room; and higher rates of post-operative adverse effects such as patient discomfort, nausea, vomiting, and longer stays in the post-anesthesia care unit. Underdosing, while less common, can lead to the serious issues of inadvertent patient awareness and potential psychological symptoms and post-traumatic stress disorder, as well as associated liability risks.2-4
In general, depth of anesthesia monitoring is associated with reduced consumption of general anesthetic drugs and decreased recovery time in comparison to clinical monitoring alone. One review indicates that depth of anesthesia monitoring may lead to reduced incidence of intraoperative hypotension and may reduce the volume of volatile anesthetic required, leading to speedier extubations and shorter time in the recovery room.4 These cost savings have the potential to offset some of the extra costs associated with implementing depth-of-anesthesia monitoring. 4,5
But beyond the benefits to the patient experience or bottom line, clinicians agree that depth of anesthesia monitoring is an essential component of patient care. According to the Association of Anaesthetists of Great Britain & Ireland, "use of depth of anaesthesia monitors, for example processed EEG monitoring, is recommended when patients are anaesthetised with total intravenous techniques and neuromuscular blocking drugs, to reduce the risk of accidental awareness during general anesthesia."7
The verdict is clear for clinicians depth of anesthesia monitoring is an essential tool for operating rooms and anesthesiologists.
References
- Marinova R, Petrova G. EEG-derived indexes for monitoring the depth of anesthesia. Vol 2.; 2018. Journal of Pain Management and Therapy. Accessed March 15, 2019.
- Nickalls RWD, Mahajan RP. Awareness and anesthesia: think dose, think data. Br J Anaesth. 2010;104(1):1-2. doi: 10.1093/bja/aep360. Accessed March 15, 2019.
- Musizza B, Ribaric S. Monitoring the depth of anesthesia. Sensors (Basel). 2010;10(12):10896-10935. doi: 10.3390/s101210896. Accessed March 15, 2019.
- Shepherd J, Jones J, Frampton G, Bryant J, Baxter L, Cooper K. Clinical effectiveness and cost-effectiveness of depth of anesthesia monitoring (E-Entropy, Bispectral Index and Narcotrend): a systematic review and economic evaluation. Health Technol Assess. 2013;17(34):1-264. doi: 10.3310/hta17340. Accessed March 15, 2019.
- El Hor T, Van Der Linden P, De Hert S, Mélot C, Bidgoli J. Impact of entropy monitoring on volatile anesthetic uptake. 2013;118(4):868-873. doi: 10.1097/ALN.0b013e3182850c36. Accessed March 16, 2019.
- Liang Z, Wang Y, Sun X, et al. EEG entropy measures in anesthesia. Front Comput Neurosci. 2015;9:16. doi: 10.3389/fncom.2015.00016. Accessed March 16, 2019.
- Association of Anaesthetists of Great Britain & Ireland. Checking Anaesthetic Equipment 2012. AAGBI Safety Guideline. London, 2012. http://www.aagbi.org/sites/default/files/checking_anaesthetic_equipment_2012.pdf (accessed 07/07/2015).