
Note: The clinical examples shown are not actual case studies but were created to illustrate how the measurements might behave given the stated conditions.
Capnometry
Easy way to follow ventilation, circulation and metabolism
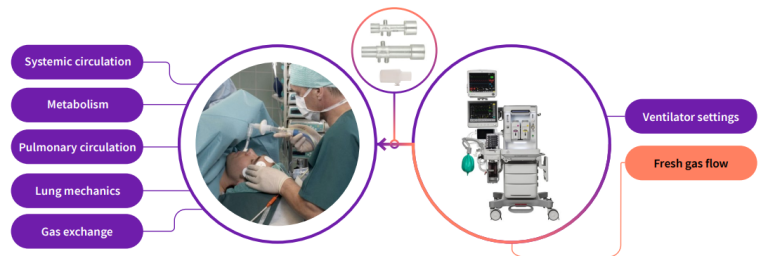
Some specific benefits of CO₂ monitoring:
- Continuous
- Non-invasive
- Easy
- May help prevent ventilator related mishaps
- Follow-up of optimized ventilation
- Rapid verification of endotracheal intubation
- Quick detection of problems in the airway or malfunction of the ventilator or gas supply
- Objective, continuous and non-invasive indicator of adequacy of ventilation
- Disturbances in gas exchange, circulation and metabolism may be easily recognized
- May help reduce the need for frequent blood gas analyses, since EtCO2 trends approximate the changes in PaCO2
Response time of various parameters to respiration-related mishaps
That table1 shows how fast detector both EtCO2 and Fi-EtO2 are in several critical situations. Even SpO2 is widely used, its response time is much slower than airway gases. SpO2 is measured on the peripheral site and EtCO2 represents the alveolar values
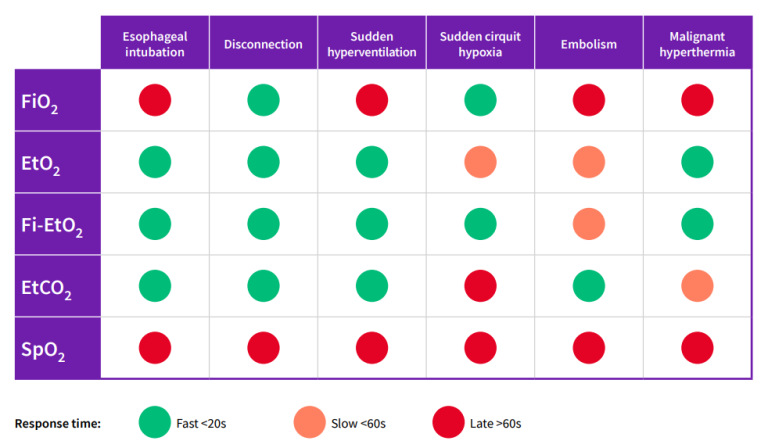
1 Stenqvist O, Paloheimo M, Meriläinen P, Paloviita P. Patient Oxygen Appliguide - your margin of safety. Datex Division Instrumentarium Corp, 1992.
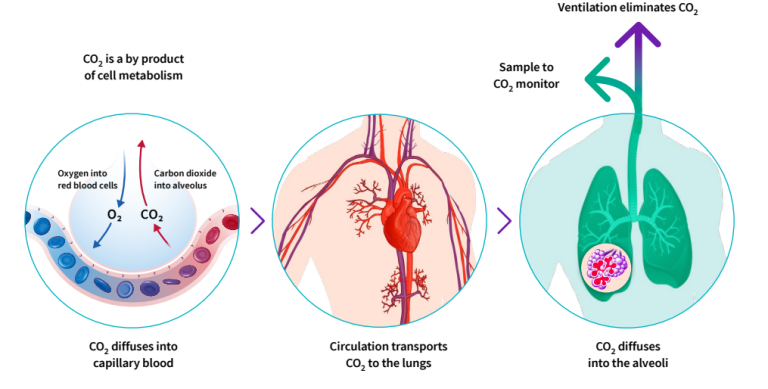
CO₂ production, transport and elimination
Oxidation of Glucose is an essential part of the energy metabolism and CO2 is a waste product which must be continually removed. From the cells carbon dioxide diffuses into the capillary blood and subsequently to the venous circulation returning blood from the periphery to the right side of the heart. When the heart contracts, the mixed venous blood is pumped through the pulmonary circulation to the lungs for gas exchange. The exhalation phase of breathing eliminates CO2 from the body. Although the lungs are by no means emptied, the final part of the exhaled gas is almost pure alveolar gas.
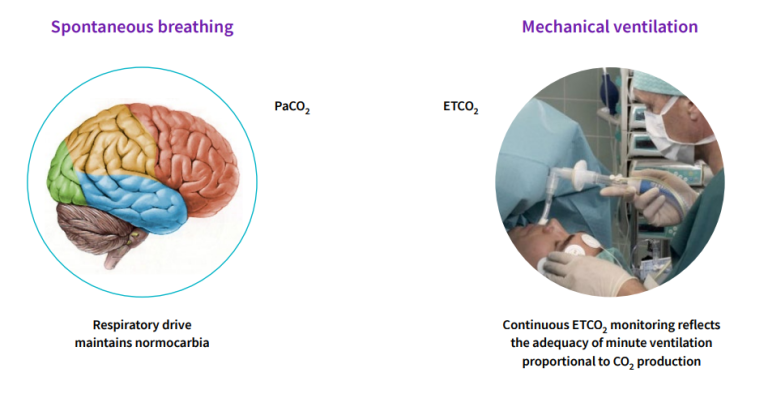
Using EtCO₂ to Control Ventilation
During spontaneous breathing, our respiratory center located in the brain, automatically regulates PaCO2 being close to 40 mmHg by increasing or decreasing the minute ventilation according to the metabolism.
During mechanical ventilation, the use of sedatives can negatively affect respiratory drive. In that case, normoventilation cannot be adequately maintained without monitoring. In the presence of neuromuscular blocking agents, spontaneous respiration ceases further illustrating the need for continuous monitoring of ventilation.
Differences in ventilation
Perioperative care

- Mostly planned operations
- Patient generally has healthy lungs
- Patients are anesthetized and often paralyzed
- No work of breathing concerns
- Short-term monitoring
Intensive care

- Very complex & started at sub-opportune times
- Many different pathologies & traumas
- Try to maintain spontaneous ventilation
- Try to keep the work of breathing to a minimum
Normal ventilation/perfusion ratio
No significant aACO₂ difference
In a healthy person with optimal ventilation-perfusion ratio aACO2 difference is 1-4 mmHg. The arterial-to-alveolar difference is due to a mismatch of ventilation and perfusion of the alveoli in the lungs. Even in healthy patients, there are some parts of the lungs which are not perfused as well as they are ventilated or vice versa.
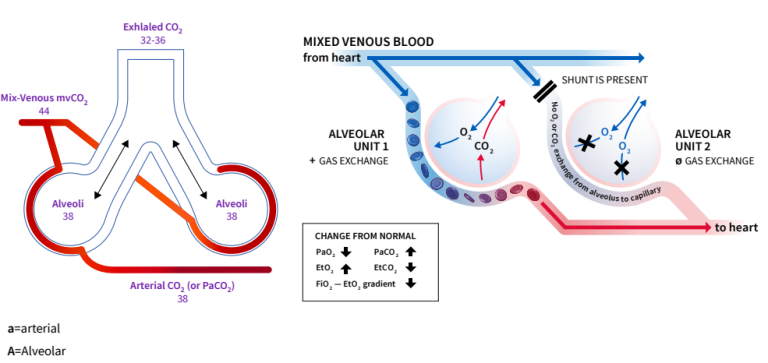
Ventilation-perfusion mismatch
Increased aACO₂ difference
Capnography provides continuous information on EtCO2, and when you compare the changes to PaCO2 (BGA) you will follow the degree of ventilation-perfusion mismatch and possibly reduce frequency of blood gas analyses.
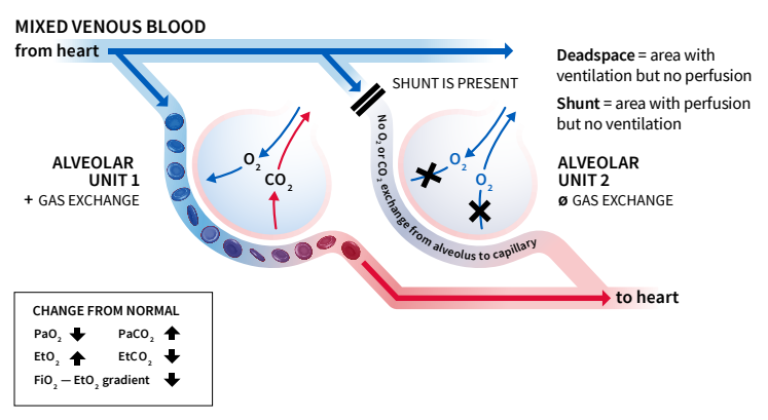
Parts of the lungs may also be well-perfused but poorly ventilated. Main reasons for shunt perfusion:
- Obstructed bronchi (mucus, foreign bodies, infection)
- Unilateral endobronchial intubation
- Increased closing volume (diaphragm pushing against the lungs)
Main reasons for dead space ventilation are:
- Pulmonary thromboembolism
- Patient position (side lying)
- Pulmonary hypoperfusion
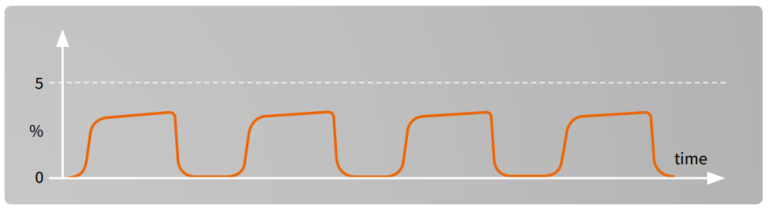
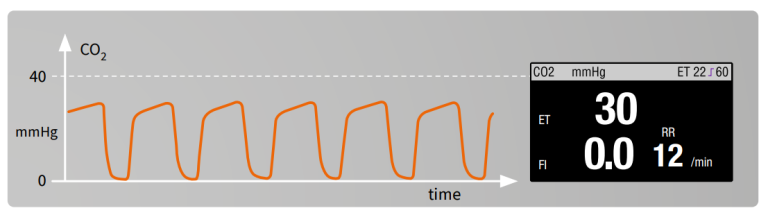
Normal capnogram
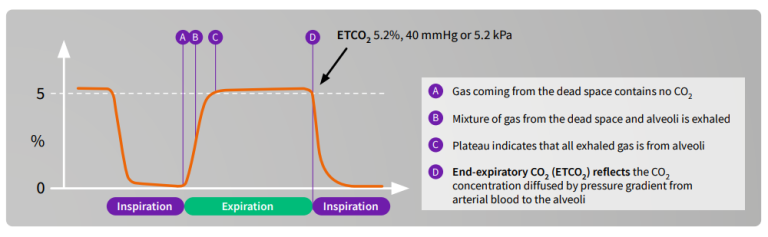
The CO2 waveform is referred to as the capnogram and it reflects the different stages in breathing. The capnogram is an important diagnostic tool because its shape is virtually identical in all basically healthy patients. Any change in shape should be investigated. EtCO2 represents the CO2 value at the end of expiration and this is typically displayed on the monitor screen.
Capnography
Normocapnia EtCO2 4.6-5.9 vol % 30-45 mmHg1
Hypocapnia EtCO2 less than 4.6 vol % 35 mmHg
Hypercapnia EtCO2 more than 5.9 vol % 45 mmHg
Common terms in CO₂ monitoring:
- ”capno” means CO2 level in breath
- ”hyper” means too much
- ”hypo” means too little
- ”carbia” refers to CO2 level in the blood
Units for measurement
The following transformation formula can be used with sufficient accuracy at normal atmospheric pressure of 760 mmHg (at sea level and at normal body temperature):
- vol % volume percentage
- mmHg partial pressure in millimeters of mercury
- kPa partial pressure in kilopascals
1 vol % = 1 kPa, 1 kPa = 7.6 mmHg, 1 mmHg = 0.13 vol%
Alveolar minute ventilation is typically adjusted to achieve normocapnia, where EtCO2 is in the range 4.6 - 5.9 vol % (35 - 45 mmHg) (at atmospheric pressure corresponding to sea level and at normal body temperature).
1 PetCO2 normal values:Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179
Benefits of normoventilation
- Maintains normal physiology
- Maintains normal cerebral perfusion1
- Spontaneous breathing reappears easily
➔ short uneventful recovery
With normoventilation, disturbances in ventilation, circulation and metabolism can be more easily recognized and monitoring enables to maintain the physiologically optimal minute ventilation. Spontaneous breathing can be instituted more easily by allowing the EtCO2 rise at the end of the anesthesia and patient usually experiences a more rapid recovery.
During lengthy anesthesia, there is typically a very gradual decrease in EtCO2 due to the depressant effect of anesthetic agents and the effect of hypothermia slowing the patient’s metabolism.
1 Z. Kalenda, Mastering Infrared Capnography, p48, 1989
Hypocapnia/Hyperventilation²
Possible reasons:
- Hyperventilation
- Decreased cardiac output
- Decreased metabolism
- Hypothermia
In anesthesia the common cause of hypocapnia is too high alveolar ventilation (hyperventilation)
In recovery or ICU hypocapnia in the spontaneously breathing patient may be result of hyperventilation due to fear, pain, failed weaning attempt or shock (circulatory failure)
Disadvantages of prolonged hyperventilation:
- Vasoconstriction leading to decreased coronary and cerebral blood flow
- Unnecessary respiratory alkalosis
- Depression of respiratory center
In specific cases there may be an advantage in hyperventilating the patient. For example, in neuroanesthesia hypocarbia may be used to deliberately reduce cerebral perfusion and intraacranial pressure.
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
Hypercapnia/Hypoventilation²
Possible reasons:
Hypoventilation
A. Spontaneous respiration
- Depression of respiratory center
- Mechanical disturbances (muscle paresis, hemo/pneumothorax, airway obstruction)
B. Artificial ventilation
- Airway obstruction
- Pneumothorax
- Leak
- Disconnection
- Over-feeding (excess calorie intake)
- Ventilator dysfunction
- Mismanagement of artificial ventilation
- Rebreathing
- Permissive hypercapnia
- Circulatory insufficiency
- Altered V/Q ratio
- Increased metabolism (e.g. burn patients)
- Bicarbonate infusion
- Compensated metabolic alkalosis depression of respiratory center
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
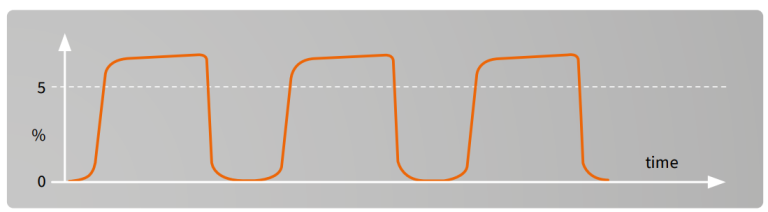
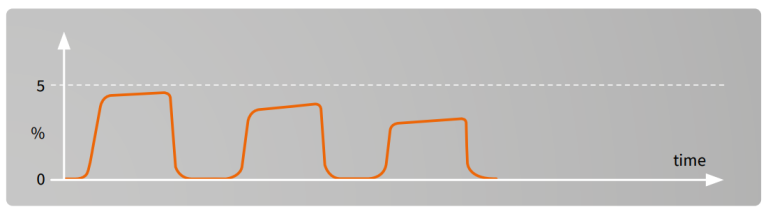
Rebreathing²
Failure of the capnogram to return to the baseline may indicate rebreathing of the exhaled CO2. This can be an inherent feature of the anesthesia delivery system (for example with Mapleson type of breathing systems) or it may be due to an exhausted CO2 absorber in a circle system. Finally, it may also be due to inadequate fresh gas flow given to the patient as set in the ventilator.
Monitoring FiO2 is the best method to determine the optimal fresh gas flow. Ref. Text book: Understanding Anesthesia equipment. 5th edition. 2008 by Lippincott Williams & Wilkins
If expiratory time is too short for CO2 curve to represent the EtCO2 value, the next inspiration will contain CO2 which can be seen as a rise in the baseline.
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
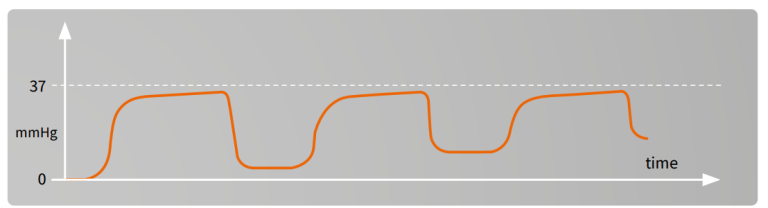
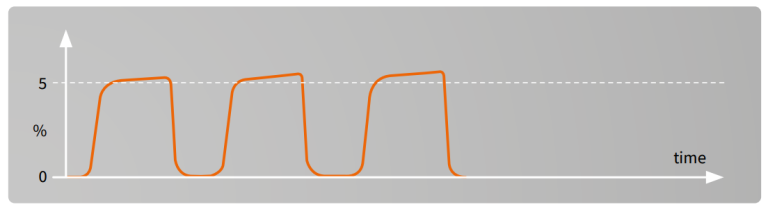
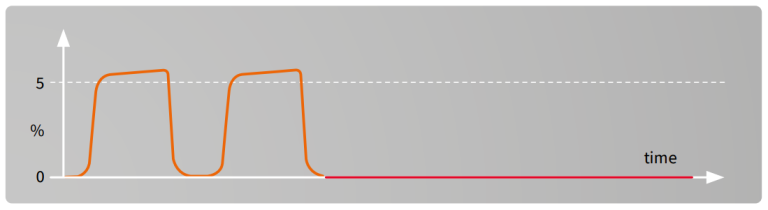
Esophageal intubation²
If intubation is difficult i.e. vocal cords are not visible, it may happen that the ET-tube is inserted accidentally into the esophagus. If this is not detected immediately the patient will die. The best indicator for early detection is capnometry.
Some CO2 may be detected due to gas entering the stomach during manual ventilation. After removal of the endotracheal tube and successful re-intubation, high EtCO2 values are recorded because of CO2 accumulation during apnea.
American Heart Association (AHA) recommends to use capnography to confirm the correct positioning of the ET-tube as well as in confirmation of the effectiveness of chest compressions during CPR.
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
Cardiac arrest and resuscitation, sudden fall to zero²
EtCO2 monitoring provides a continuous information in detecting return of spontaneous circulation during cardiac resuscitation.
American Heart Association (AHA) recommends to use capnography to confirm the correct positioning of the ET-tube as well as in confirmation of the effectiveness of chest compressions during CPR.
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
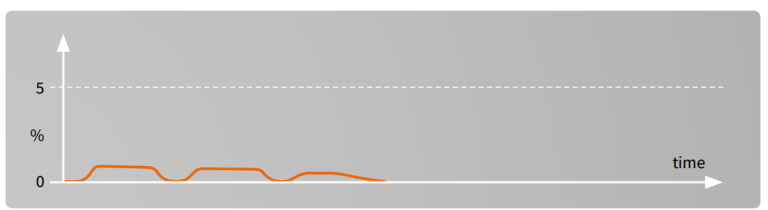
Vasopressors, bicarbonate, tourniquet²
Sudden but transient rise in ETCO2 while inspired CO2 remains zero may be due to the release of a tourniquet or infusion of bicarbonate.
Some orthopedic operations are performed using tourniquet in order to get the surgical field bloodless. The use of tourniquet will lead to ischemic reaction in the limb and after the release of tourniquet the acidotic substance will be released into the circulation. This effect can be seen as transient rise in ETCO2.
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
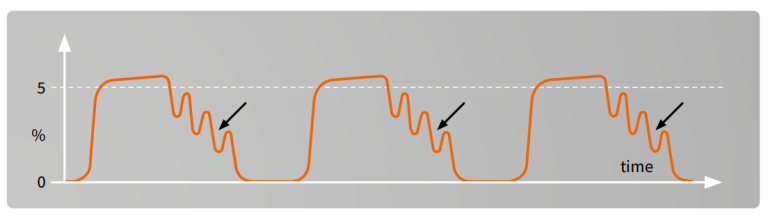
Efforts of spontaneous breaths²
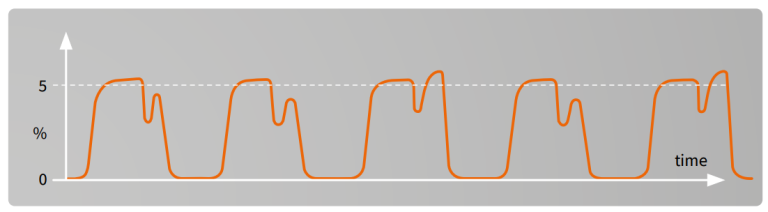
Insufficient muscular relaxation and/or inadequate depth of anesthesia are allowing the patient ”fight” against the mechanical ventilation. These shallow, efforts of spontaneous breaths can be seen as clefts on the capnogram plateau.
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
Partially obstructed airway²
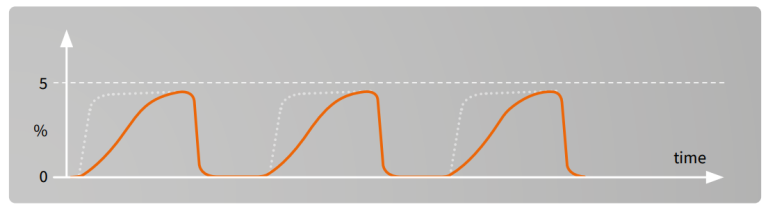
Possible causes:
- Secretions
- Bronchospasm
- Kink of ET-tube
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
Sudden disappearance of CO₂ waveform²
Possible reasons:
- Ventilator disconnection
- Totally obstructed ET-tube
- Gas sampling line disconnected
- Cardiac arrest
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
Sudden decrease of ETCO₂²
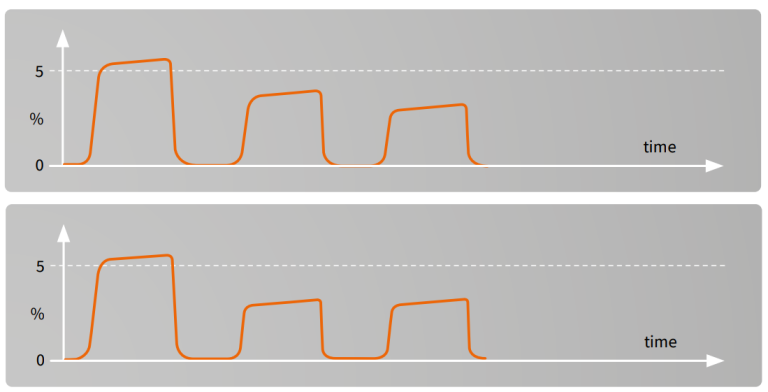
A rapid fall in ETCO₂ over a period of several breaths may indicate:
- Pulmonary embolism
- Cardiac arrest
- Severe hypotension (massive bleeding)
- Leak in sampling system
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
Cardiogenic oscillations²
Possible reasons:
- Continuous gas flow fed directly into the inspiratory limb
- Side stream gas sampling taken at the Y-peace
- Slow respiration rate
- Long expiration time
2 PetCO2 normal values: Variables Associated with EtCO₂ Values. Prehospital Emergency Care, 16(2): 250-256. Tobin, M. J., & Grenvik, A. (1984). Monitoring of the Patient in the Intensive Care Unit. New England Journal of Medicine, 310(18): 1170-1179. https://www.jems.com/2017/08/01/how-to-read-and-interpret-end-tidal-cap… https://www.capnography.com/
Sample flow rate effect
- Table presents different sampling volumes depending on respiration rate
- The I:E ratio is assumed to be 1:2
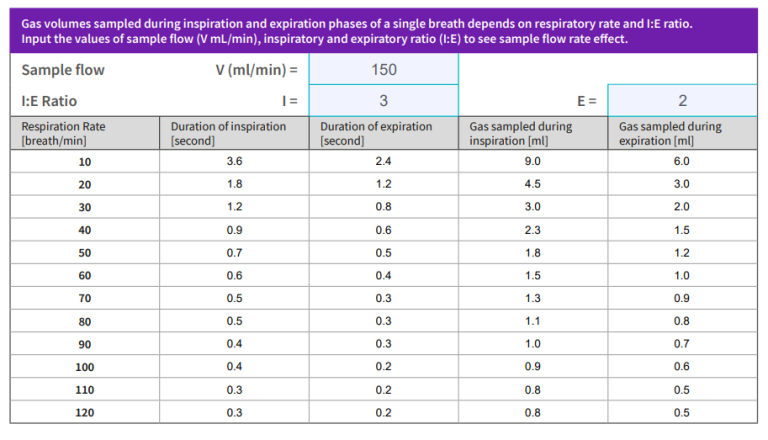
Note: You can change the sample flow/min and I:E ratio values to see how the sampled gas is distributed per breathing cycle
The effect of the sample flow rate by the side stream analyzer is seen in the table. The amount of gas drawn by the monitor is dependent on the respiratory rate. When the respiratory rate increases the sample gas will decrease by breath. Also the total volume sampled is devided between the inspiration and expiration.
Example: with a respiration of 30, which may be common for small babies, the total volume sampled is 4 ml only, where 1,3 ml is drawn during the inspiration. This makes the 120 ml flow rate feasible for small babies as well.
Clinical benefits
Patient safety
- Confirms the correct place of ET-tube
- Continuous measurement to detect hyperventilation or hypoventilation quickly
- Estimation of increased/decreased shunt
- ETCO2 trend vs PaCO2
Optimal minute ventilation=normoventilation
Suggested reading
Brast, S., Bland, E., Jones-Hooker, C., Long, M., and Green, K. (2016). Capnography for the Radiology and Imaging Nurse: A Primer. Journal of Radiology Nursing, Volume 35, Issue 3, 173 – 190
Kodali, B. S. (2013). “Capnography Outside the Operating Rooms.” Anesthesiology: The Journal of the American Society of Anesthesiologists, 118(1): 192-201.
Brunetti, M. A., Santarelli, G., & Berrio, C. S. (2009). “Capnography in Emergency Medicine.”Journal of Emergency Medicine, 37(2): 239-245.
Ehrman, R. R., Guyette, F. X., & Ashton, J. A. (2012). “Capnography in Out-of-Hospital Cardiac Arrest
J. S. Gravenstein, M. B. Jaffe, N. Gravenstein, D. A. Paulus: Capnography. Text book
Capnography, Second Edition, Anesthesiology 3 2012, Vol.116, 744-745.
Rationales and Applications for Capnography, Monitoring During Sedation, Devin Carr, MSN, MS, RN, RRT, ACNS-BC, NEA-BC, CPPS and Anna Cartwright, BSN; RNClinicalfoundations.org
End-Tidal Capnography Updated: Jan 17, 2020. Author: Robert Thomas Arrigo, MD, MS; Chief Editor: Zab Mosenifar, MD, FACP, FCCP
How to Read and Interpret End-Tidal Capnography Waveforms For additional clinical resources, please visit clinicalview.gehealthcare.com
For additional clinical resources, please visit clinicalview.gehealthcare.com
Not all products or features are available in all markets. Full product technical specification is available upon request. Contact a GE HealthCare Representative for more information. Please visit www.gehealthcare.com.
Data subject to change.
© 2025 GE HealthCare
GE is a trademark of General Electric Company used under trademark license.
Reproduction in any form is forbidden without prior written permission from GE HealthCare. Nothing in this material should be used to diagnose or treat any disease or condition. Readers must consult a healthcare professional.
JB35961XX_JB16327XX_1 4/2025








