Quantitative neuromuscular monitoring and the reduction of residual neuromuscular block¹
Under-recognized post operative residual paralysis2,5,6
of cases do not reach 90%² train-of-four (TOF) ratio extubation threshold, leading to insufficient neuromuscular recovery¹
40-83%
May lead to increased mortality
Unreliable visual and tactile assessment of neuromuscular function1,2
Subjective and healthcare provider dependent evaluation
Neuromuscular block with TOF > 40% canʼt be reliably detected even by experienced anaesthetists²
Evaluations that lead to misinterpretation of adequate recovery²

Ability to lift the head

Sufficient minute ventilation of an intubated patient
Patients can lift the head and hold firm handshake for five seconds with TOFR = 0.33²
Normal vital capacity possible with
TOFR = 0.6²
Quantitative neuromuscular monitoring to accurately assess neuromuscular block
One of the only suitable methods
To titrate adequate levels of neuromuscular block
To guide optimal dose and timing of reversal agent

Recommended by
ESAIC, ASA & APSF
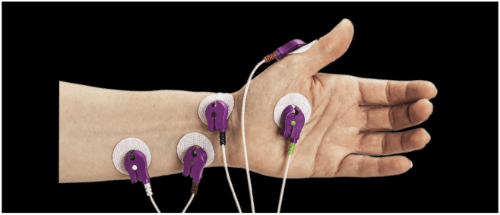
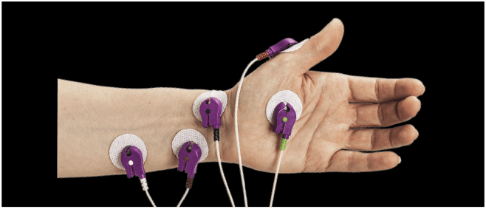
Electromyography (EMG) is the gold standard for measuring neuromuscular block¹
Offers advantages versus other technologies
Captures the first clean signal at the neuromuscular junction
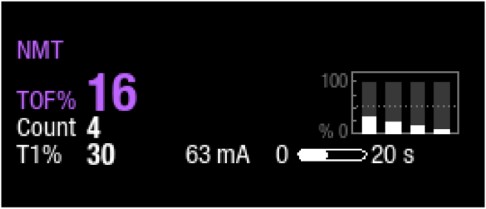
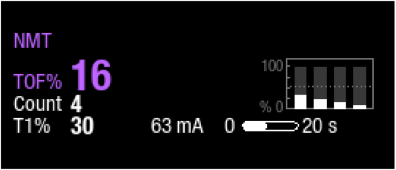
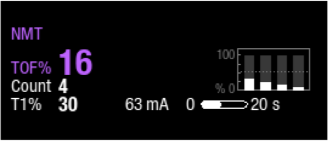
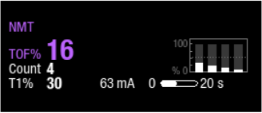
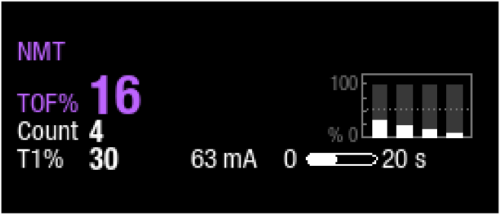
TOF*
Four stimulation pulses are generated at 0.5 sec intervals. The response is measured after
each stimulus, and the ratio of the fourth to the first response of the TOF sequence is calculated,
resulting in TOF%.

PTC**
Tetanic stimulation is a continuous 5 sec stimulation. After tetanic stimulation, single
twitch stimulations are generated. The number of detected responses is counted and expressed as PTC.
The fewer the responses, the deeper the relaxation.
*TOFC = number of elicited contractions
TOFR = ratio of 4th to 1st
twitch response
**PTC is used if there is no response to TOF or a single twitch (i.e. in profound
non-depolarising block)
Quantitative neuromuscular monitoring to support reversal agent choice and dose decision2,4
With TOF <90 residual neuromuscular block is present and has to be reversed by either waiting or by administering reversal drugs
Correct choice of dose, timing and reversal drug are crucial for achieving complete neuromuscular recovery and allow safe extubation
measurement
TOFC = 4
TOFR < 0.2
(μg/kg)
(mga/kg)






Optimal dose and injection
time of reversal agent¹

Increased likelihood of complete neuromuscular
recovery⁵

experience⁶
throughput²
*These doses have been determined in dose-finding studies, and have not been tested in comparative clinical trials. They are not recommended by the manufacturer. Please note that the use of low-dose sugammadex has been questioned, since elderly patients are at greater risk for recurarisation and residual muscle paralysis when low-dose sugammadex is administered.
Naguib M, Brull SJ, Kopman AF, Hunter JM, Fulesdi B, Arkes HR, Elstein A, Todd MM, Johnson KB. Consensus Statement on Perioperative Use of Neuromuscular Monitoring. Anesth Analg 2018;127:71-80.
Blobner M, Eikermann E, Lewald H. Safe and Efficient Anesthesia: The Role of Quantitative Neuromuscular Monitoring. Advances in Patient Safety.
Viby-Mogensen J, Jensen NH, Engbaek J, Ording H, Skovgaard LT, Chraemmer-Jorgensen B. Tactile and visual evaluation of the response to train-of-four nerve stimulation. Anesthesiology 1985;63:440-443.
Sasakawa T, Miyasaka K, Sawa T, Iida H. Postoperative Recurarization After Sugammadex Administration Due to the Lack of Appropriate Neuromuscular Monitoring: The Japanese Experience’. APSF Newsletter. 2020:42-43.
Todd M, Hindman B, King B. The Implementation of Quantitative Electromyographic Neuromuscular Monitoring in an Academic Anesthesia Department. Anesth Analg 2014:119 Number 2:323-331.
Benoît Plaud, Bertrand Debaene, François Donati, Jean Marty. Residual Paralysis after Emergence from Anesthesia, Anesthesiology 2010;1013-1022.
Not all products or features are available in all markets. Full product technical specification is available
upon request. Contact a GE HealthCare Representative for more information. Please visit
www.gehealthcare.com/promotional-locations. Data subject to change.
© 2023 GE HealthCare
GE is a
trademark of General Electric Company used under trademark license. All other trademarks are property of
their respective owners.
Reproduction in any form is forbidden without prior written permission from GE
HealthCare. Nothing in this material should be used to diagnose or treat any disease or condition. Readers
must consult a healthcare professional.
JB02095XX-JB27114XX 12/2023